Papillary renal cell carcinoma (PRCC) is a distinct type of kidney cancer that accounts for approximately 15-20% of all renal cell carcinomas. This unique form of kidney cancer requires specialized understanding and treatment approaches, making early detection and proper diagnosis crucial for optimal outcomes.
Understanding the characteristics, symptoms, and treatment options for papillary renal cell carcinoma can help patients and healthcare providers make informed decisions about care and management strategies. This comprehensive guide explores the essential aspects of PRCC, including its various types, diagnostic methods, and current treatment approaches.
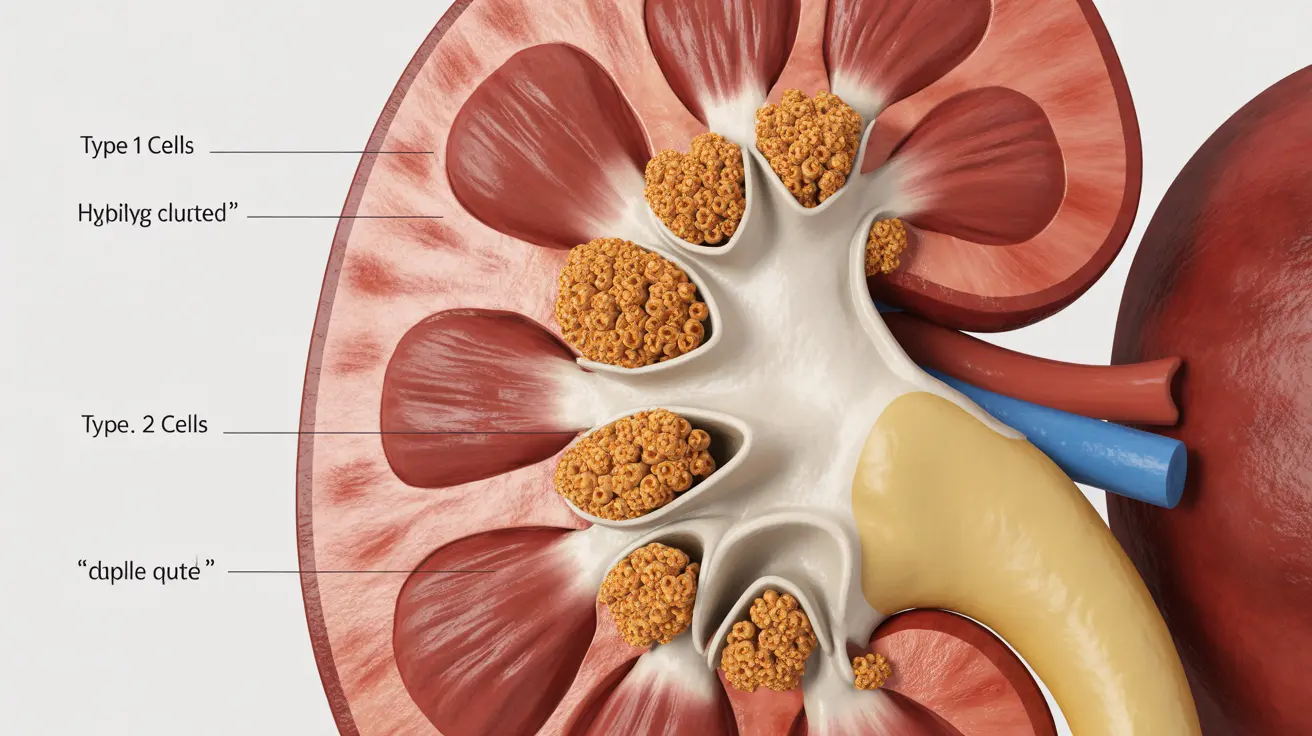
Key Characteristics and Types
Papillary renal cell carcinoma is characterized by its distinctive growth pattern, forming finger-like projections called papillae. The disease is classified into two main subtypes, each with unique features and prognosis:
Type 1 PRCC
Type 1 PRCC typically presents with:
- Small cells arranged in a single layer
- Better prognosis compared to Type 2
- More common in patients with hereditary kidney cancer syndromes
- Generally slower growth rate
Type 2 PRCC
Type 2 PRCC characteristics include:
- Larger cells with abundant cytoplasm
- More aggressive behavior
- Generally poorer prognosis
- Higher likelihood of metastasis
Early Detection and Symptoms
Early detection of papillary renal cell carcinoma can be challenging as symptoms may not appear until the disease has advanced. Common symptoms include:
- Blood in urine (hematuria)
- Persistent back or flank pain
- Unexplained weight loss
- Fatigue
- Abdominal mass or swelling
- High blood pressure (in some cases)
Diagnostic Procedures
Diagnosis of papillary renal cell carcinoma typically involves multiple steps and imaging techniques:
- CT scans with contrast
- MRI imaging
- Ultrasound examination
- Kidney biopsy (when necessary)
- Blood and urine tests
- Genetic testing (particularly in cases with family history)
Treatment Approaches
Treatment strategies for papillary renal cell carcinoma vary depending on several factors, including:
Surgical Options
- Partial nephrectomy (removal of tumor while preserving kidney function)
- Radical nephrectomy (complete kidney removal)
- Minimally invasive surgical techniques when appropriate
Targeted Therapies
- MET inhibitors for specific genetic mutations
- Antiangiogenic drugs
- Immunotherapy options
- Clinical trial participation opportunities
Risk Factors and Prevention
Understanding risk factors can help with prevention and early detection:
- Advanced age
- Male gender
- Smoking history
- Obesity
- Family history of kidney cancer
- Certain genetic conditions
- Chronic kidney disease
Frequently Asked Questions
What are the common symptoms and early signs of papillary renal cell carcinoma?
Common symptoms include blood in urine, flank pain, unexplained weight loss, and fatigue. However, many patients may be asymptomatic in early stages, with tumors discovered incidentally during imaging for other conditions.
How is papillary renal cell carcinoma diagnosed and staged?
Diagnosis involves imaging studies (CT, MRI, ultrasound), possible biopsy, and comprehensive blood work. Staging considers tumor size, lymph node involvement, and presence of metastasis using the TNM classification system.
What are the differences between Type 1 and Type 2 papillary renal cell carcinoma?
Type 1 PRCC typically has better outcomes, with small cells arranged in a single layer and slower growth. Type 2 PRCC is more aggressive, features larger cells, and generally has a poorer prognosis.
What treatment options are available for papillary renal cell carcinoma, including surgery and targeted therapies?
Treatment options include surgical removal (partial or radical nephrectomy), targeted therapies like MET inhibitors, immunotherapy, and participation in clinical trials. The choice depends on cancer stage, patient health, and specific genetic markers.
What are the risk factors and causes associated with developing papillary renal cell carcinoma?
Risk factors include advanced age, male gender, smoking, obesity, family history of kidney cancer, certain genetic conditions, and chronic kidney disease. Some cases may be linked to specific genetic mutations.