Living with Parkinson's disease presents various challenges, and one significant but often under-discussed aspect is urinary incontinence. This common symptom can significantly impact quality of life, affecting both daily activities and social interactions. Understanding the connection between Parkinson's and incontinence is crucial for better management and maintaining independence.
How Parkinson's Disease Affects Bladder Function
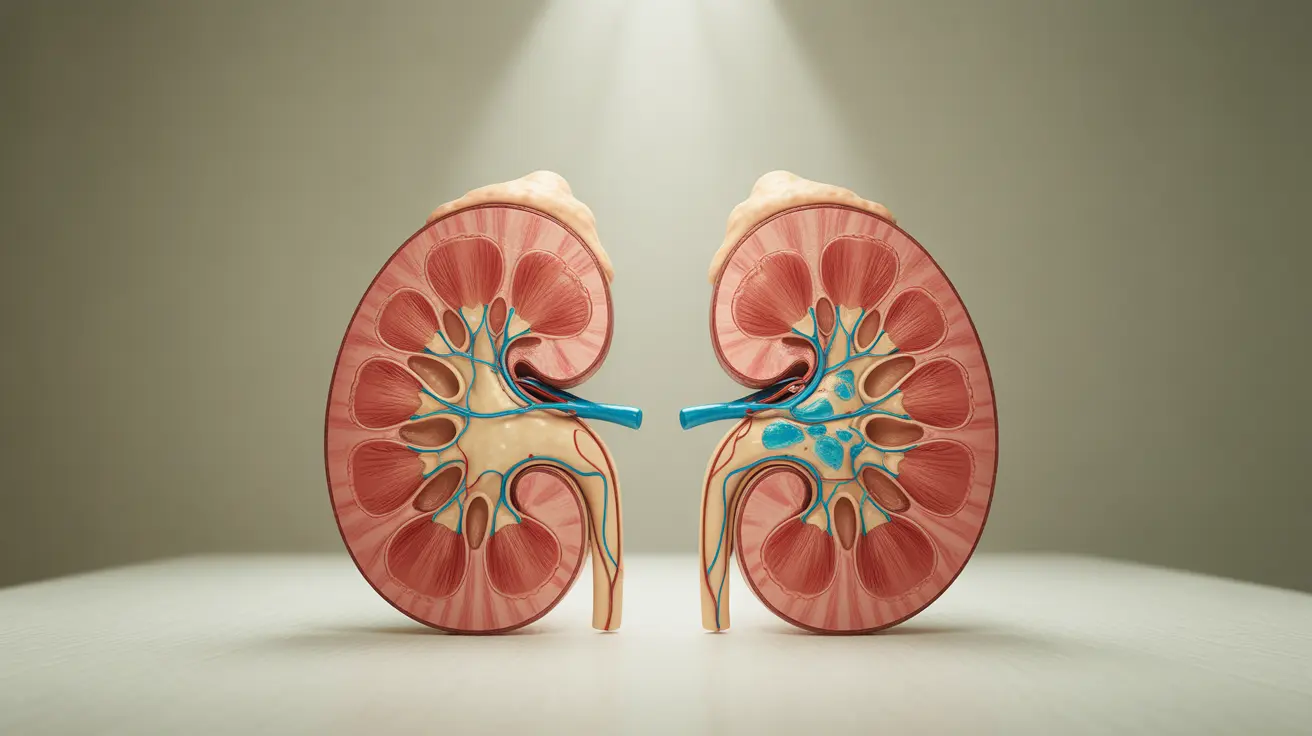
Parkinson's disease can directly impact the nervous system's control over bladder function. The condition affects nerve signals between the brain and bladder, leading to various urinary symptoms. These disruptions can cause both storage and emptying problems, making bladder control increasingly challenging as the disease progresses.
Common Bladder Issues in Parkinson's Disease
People with Parkinson's often experience several types of urinary problems:
- Urgency: Sudden, intense urges to urinate
- Frequency: Needing to urinate more often than usual
- Nocturia: Increased nighttime urination
- Incomplete emptying: Difficulty fully emptying the bladder
- Stress incontinence: Leakage during physical activities
Impact of Parkinson's Medications on Bladder Control
Medications used to treat Parkinson's disease can have varying effects on bladder function. While some medications may help improve motor symptoms, they might inadvertently affect bladder control. Understanding these medication effects is crucial for developing an effective management strategy.
Medication Side Effects and Adjustments
Common Parkinson's medications can either improve or worsen bladder symptoms. Working closely with healthcare providers to find the right balance between managing motor symptoms and bladder control is essential. Medication timing and dosage adjustments may help minimize adverse effects on bladder function.
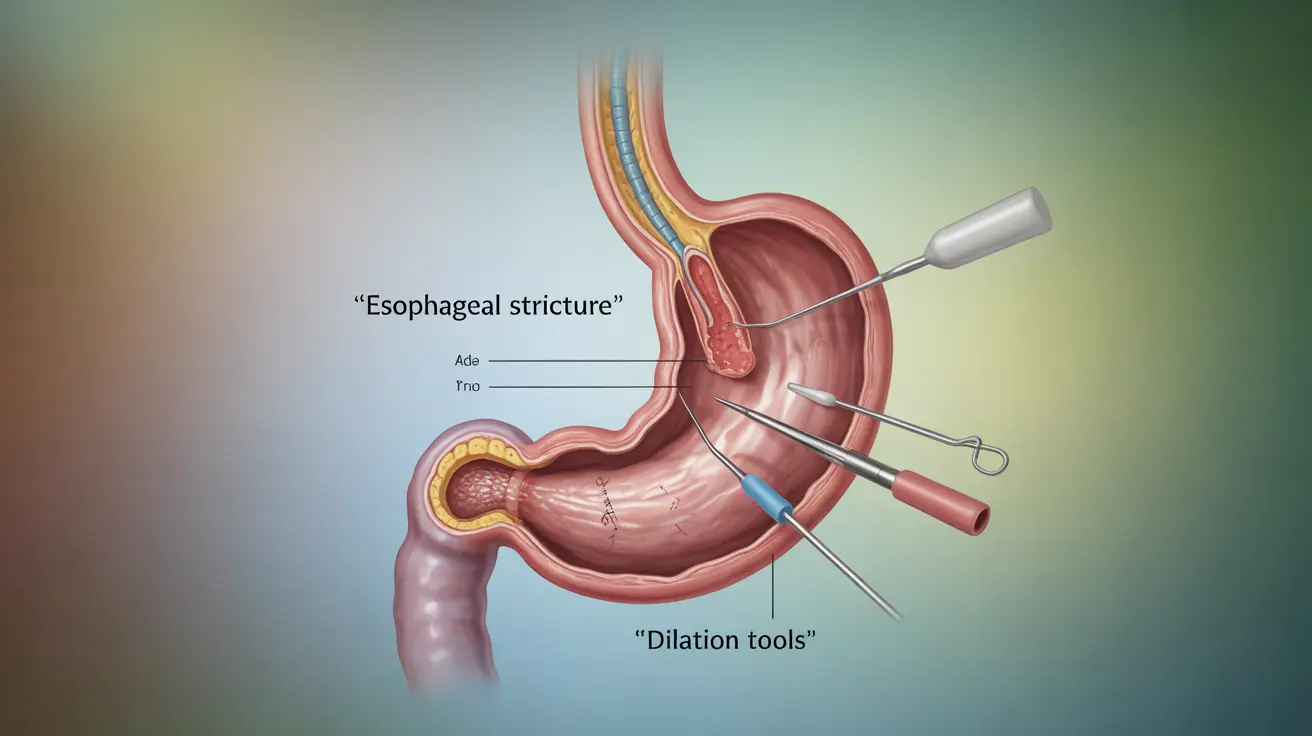
Treatment Options for Urinary Symptoms
Several treatment approaches can help manage incontinence in Parkinson's disease:
- Medications specifically for bladder control
- Pelvic floor exercises
- Bladder training techniques
- Lifestyle modifications
- Medical devices and supports
- Surgical interventions in severe cases
Working with Healthcare Providers
A comprehensive treatment plan often involves collaboration between neurologists, urologists, and other specialists. Regular monitoring and adjustment of treatments ensure optimal management of both Parkinson's symptoms and bladder control issues.
Lifestyle Management Strategies
Effective management of urinary symptoms often involves practical lifestyle changes:
- Maintaining a consistent bathroom schedule
- Planning fluid intake throughout the day
- Making environmental modifications for easier bathroom access
- Using appropriate incontinence products
- Wearing easily manageable clothing
Frequently Asked Questions
What are the most common bladder problems people with Parkinson's disease experience, and how do they affect daily life? The most common bladder problems include frequent urination, urgent needs to urinate, difficulty initiating urination, and incomplete bladder emptying. These symptoms can significantly impact daily activities, sleep quality, and social interactions.
How do Parkinson's medications impact bladder control, and what are the common side effects? Parkinson's medications can affect bladder function in various ways. Some medications may increase urinary frequency or urgency, while others might help improve bladder control. Side effects can include increased or decreased urination, and medication timing can impact symptom management.
What are some effective treatments for urinary incontinence in Parkinson's patients, and when might a urologist be consulted? Effective treatments include medications for overactive bladder, pelvic floor exercises, and bladder training. A urologist should be consulted when symptoms significantly impact quality of life, when initial treatments aren't effective, or when complications develop.
Can changes in diet or lifestyle help manage urinary symptoms in Parkinson's disease, and what role does hydration play? Yes, dietary and lifestyle changes can help manage symptoms. Proper hydration timing, avoiding bladder irritants, and maintaining a regular bathroom schedule can improve control. Balanced hydration is crucial - too little can cause urinary tract infections, while too much can worsen frequency.
How does Parkinson's disease progression affect the likelihood and severity of urinary incontinence over time? As Parkinson's disease progresses, urinary symptoms often become more pronounced. The likelihood and severity of incontinence typically increase due to advancing nervous system changes and reduced mobility, making proactive management strategies increasingly important.