Pelvic floor muscle dysfunction is a common yet often misunderstood condition that can significantly impact quality of life for both men and women. This complex disorder affects the muscles, ligaments, and connective tissues that support the pelvic organs and control bladder and bowel function. Understanding its symptoms, causes, and treatment options is crucial for effective management and recovery.
Whether you're experiencing symptoms or seeking preventive information, this comprehensive guide will help you understand pelvic floor muscle dysfunction and the various approaches to treatment and management.
Understanding Pelvic Floor Muscle Dysfunction
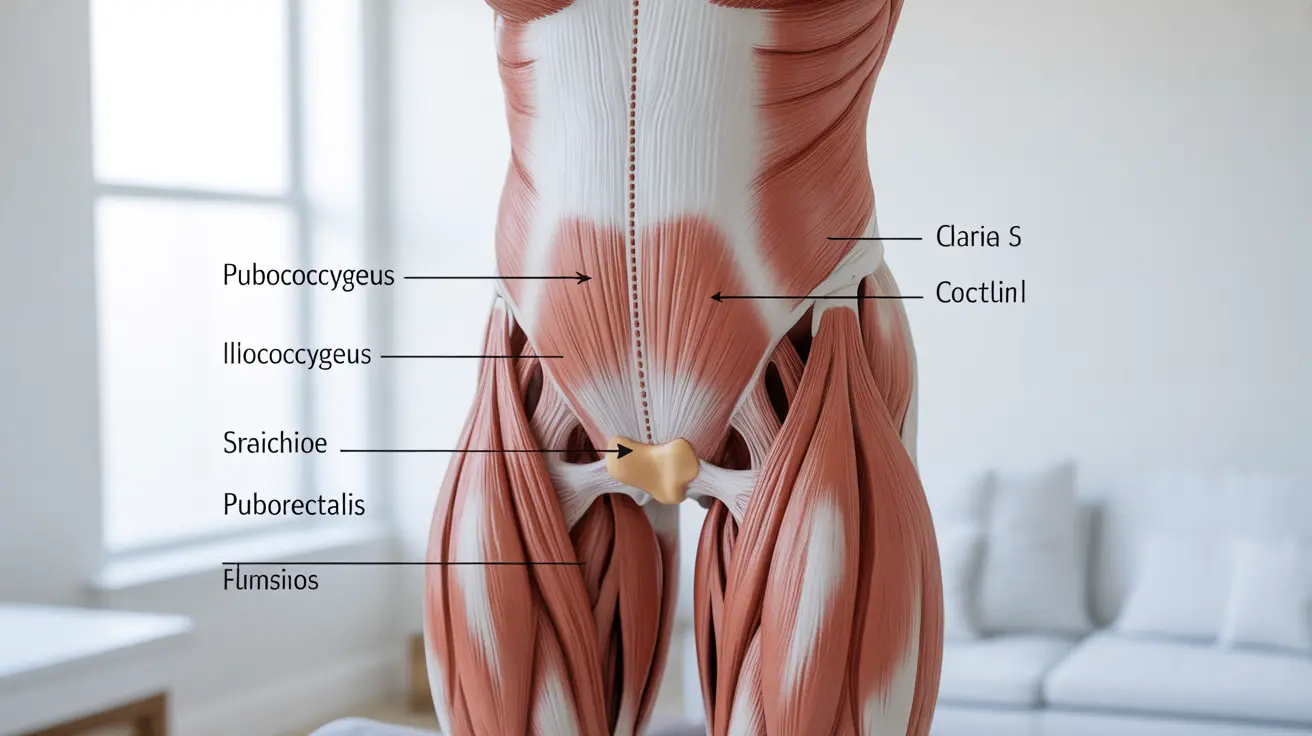
Pelvic floor muscle dysfunction occurs when the pelvic floor muscles become too weak, too tight, or have difficulty coordinating proper movement. These muscles play a crucial role in supporting pelvic organs, maintaining continence, and contributing to sexual function.
Common Symptoms and Warning Signs
The symptoms of pelvic floor muscle dysfunction can vary significantly between individuals and may include:
- Difficulty with bladder control or frequent urination
- Constipation or bowel movement difficulties
- Pelvic pain or pressure
- Lower back pain
- Pain during sexual activity
- Feeling of heaviness or fullness in the pelvic region
- Muscle spasms in the pelvic area
Risk Factors and Causes
Several factors can contribute to the development of pelvic floor muscle dysfunction:
Physical Factors
- Pregnancy and childbirth
- Surgery in the pelvic region
- Chronic coughing
- Heavy lifting
- Obesity
- Age-related changes
Medical Conditions
- Neurological disorders
- Chronic constipation
- Endometriosis
- Prostate conditions in men
Diagnosis and Assessment
Healthcare providers use various methods to diagnose pelvic floor muscle dysfunction:
- Physical examination
- Medical history review
- Muscle strength testing
- Internal examination when necessary
- Imaging studies in some cases
- Surface EMG testing
Treatment Approaches
Physical Therapy Interventions
Physical therapy is often the first-line treatment for pelvic floor muscle dysfunction. Common therapeutic approaches include:
- Targeted exercise programs
- Biofeedback training
- Manual therapy techniques
- Relaxation techniques
- Education on proper muscle coordination
Additional Treatment Options
Other treatment modalities may include:
- Medications for pain management
- Electrical stimulation therapy
- Behavioral modifications
- Stress reduction techniques
- Lifestyle adjustments
Prevention and Self-Care Strategies
Several lifestyle modifications can help prevent or manage pelvic floor muscle dysfunction:
- Maintaining a healthy weight
- Proper lifting techniques
- Regular exercise with appropriate form
- Good posture habits
- Adequate hydration
- Balanced diet
- Stress management
Frequently Asked Questions
What are the common symptoms of pelvic floor muscle dysfunction in men and women?
Common symptoms include urinary problems, bowel difficulties, pelvic pain, sexual dysfunction, and a feeling of pressure or heaviness in the pelvic region. Men may experience additional prostate-related symptoms, while women might experience vaginal symptoms or prolapse sensations.
What causes pelvic floor muscle dysfunction and who is at risk?
The condition can be caused by pregnancy, childbirth, surgery, aging, obesity, chronic straining, and certain medical conditions. Those at higher risk include pregnant women, individuals who've had pelvic surgery, athletes performing high-impact activities, and people with chronic conditions affecting the pelvic region.
How is pelvic floor muscle dysfunction diagnosed by doctors?
Diagnosis typically involves a comprehensive physical examination, detailed medical history, and assessment of muscle strength and coordination. Doctors may also use specialized tests like EMG studies or imaging to confirm the diagnosis and determine the extent of dysfunction.
What non-surgical treatments and physical therapies are effective for pelvic floor muscle dysfunction?
Effective non-surgical treatments include pelvic floor physical therapy, biofeedback training, manual therapy, electrical stimulation, and therapeutic exercises. These approaches are often combined with lifestyle modifications and behavioral techniques for optimal results.
Can lifestyle changes and exercises help prevent or reduce symptoms of pelvic floor muscle dysfunction?
Yes, lifestyle modifications such as maintaining a healthy weight, proper exercise technique, good posture, and regular pelvic floor exercises can help prevent and manage symptoms. Stress reduction and proper toileting habits also play important roles in prevention and management.