Experiencing a period every two weeks during perimenopause can be both physically exhausting and emotionally concerning. This dramatic shift in your menstrual cycle is actually one of the most common symptoms women face as they transition toward menopause, affecting up to 90% of women during this life stage.
Understanding why these frequent periods occur and knowing when to seek medical attention can help you navigate this challenging phase with greater confidence and peace of mind. While irregular bleeding patterns are typically normal during perimenopause, recognizing the difference between expected changes and potential red flags is essential for maintaining your health.
Understanding Perimenopause and Menstrual Changes
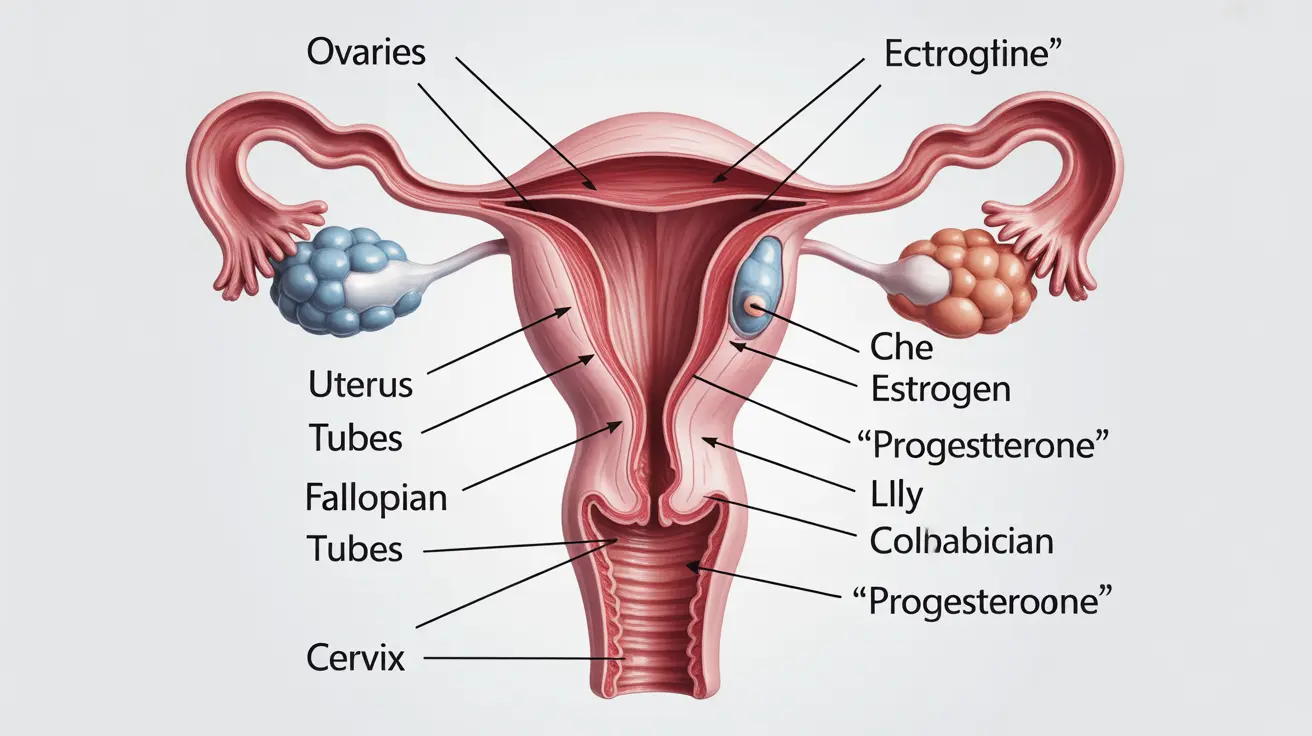
Perimenopause represents the transitional period leading up to menopause, typically beginning in a woman's 40s but sometimes starting as early as the mid-30s. During this phase, your ovaries gradually produce less estrogen and progesterone, creating significant hormonal fluctuations that directly impact your menstrual cycle.
These hormonal shifts can manifest in various ways, with frequent periods being one of the most disruptive symptoms. Your body is essentially recalibrating its reproductive system, which explains why cycles that were once predictable may suddenly become erratic and more frequent.
The Science Behind Shorter Cycles
When periods occur every two weeks, it often indicates a shortened luteal phase – the time between ovulation and menstruation. Declining progesterone levels during perimenopause can cause this phase to compress from the typical 12-14 days to as few as 7-8 days, resulting in cycles that range from 14-21 days instead of the standard 28-day cycle.
Root Causes of Frequent Perimenopause Bleeding
Multiple factors contribute to the development of frequent periods during perimenopause, with hormonal imbalance being the primary driver. As estrogen levels fluctuate unpredictably and progesterone production decreases, your endometrium (uterine lining) may thicken and shed more irregularly.
Anovulatory cycles – menstrual periods without ovulation – become increasingly common during perimenopause. When ovulation doesn't occur, progesterone isn't produced, leading to estrogen dominance that can cause the uterine lining to build up excessively and shed unpredictably.
Additional Contributing Factors
Beyond hormonal changes, several other factors can exacerbate frequent bleeding during perimenopause:
- Stress and lifestyle factors that further disrupt hormone production
- Weight fluctuations that affect estrogen levels
- Thyroid disorders that commonly emerge during this life stage
- Certain medications that interfere with hormonal balance
- Underlying conditions such as fibroids or polyps that become more problematic with hormonal changes
Recognizing Normal vs. Concerning Symptoms
While frequent periods are common during perimenopause, certain symptoms warrant immediate medical attention. Normal perimenopausal bleeding typically involves changes in cycle length, flow intensity, and duration, but should still allow you to manage daily activities with appropriate menstrual products.
Heavy bleeding that soaks through a pad or tampon every hour for several consecutive hours, bleeding that lasts longer than seven days, or bleeding accompanied by severe cramping may indicate underlying conditions requiring treatment. Additionally, any bleeding between periods or after intercourse should be evaluated by a healthcare provider.
Warning Signs Requiring Medical Evaluation
Contact your healthcare provider if you experience bleeding that significantly impacts your quality of life, causes anemia symptoms like fatigue and weakness, or occurs alongside other concerning symptoms such as severe pelvic pain or unexplained weight changes.
Effective Management Strategies
Managing frequent periods during perimenopause requires a multifaceted approach addressing both immediate symptoms and long-term health considerations. Lifestyle modifications often provide the foundation for successful management, including maintaining a balanced diet rich in iron to prevent anemia and engaging in regular exercise to help regulate hormones.
Tracking your cycles using a period tracking app or calendar can help identify patterns and provide valuable information for your healthcare provider. This documentation becomes particularly important when determining whether treatment interventions are necessary.
Medical Treatment Options
When lifestyle modifications aren't sufficient, several medical treatments can help regulate frequent periods during perimenopause. Hormonal contraceptives, including birth control pills, patches, or intrauterine devices, can provide cycle control while offering contraceptive benefits during this still-fertile period.
Non-hormonal options include anti-inflammatory medications that can reduce heavy bleeding and tranexamic acid, which helps blood clot more effectively. For severe cases, minimally invasive procedures such as endometrial ablation may be considered to reduce menstrual flow.
Long-term Health Considerations
Frequent periods during perimenopause can lead to iron deficiency anemia if left unmanaged, making it essential to monitor your iron levels and consider supplementation when appropriate. Regular check-ups with your healthcare provider ensure that any underlying conditions contributing to irregular bleeding are identified and treated promptly.
Maintaining bone health becomes increasingly important during perimenopause, as declining estrogen levels can accelerate bone loss. Adequate calcium and vitamin D intake, along with weight-bearing exercise, help preserve bone density during this transitional period.
Frequently Asked Questions
Can perimenopause cause periods every 2 weeks?
Yes, perimenopause can absolutely cause periods every two weeks. This occurs due to declining progesterone levels that shorten the luteal phase of your cycle, creating cycles as short as 14-21 days. This pattern is particularly common in early perimenopause when hormone levels are fluctuating most dramatically.
Why are my periods coming closer together during perimenopause?
Periods come closer together during perimenopause primarily because of hormonal imbalances, specifically declining progesterone and fluctuating estrogen levels. These changes can shorten your overall cycle length, reduce the time between ovulation and menstruation, and create anovulatory cycles that occur more frequently than normal ovulatory cycles.
What causes irregular periods and frequent bleeding in perimenopause?
Irregular periods and frequent bleeding during perimenopause result from erratic hormone production as your ovaries begin shutting down. Fluctuating estrogen levels cause unpredictable thickening of the uterine lining, while decreased progesterone leads to irregular shedding patterns. Additional factors like stress, weight changes, and underlying conditions can further contribute to irregular bleeding.
When should I see a doctor about frequent or heavy periods during perimenopause?
You should see a doctor if your periods occur more frequently than every 21 days, last longer than seven days, require changing protection every hour for several consecutive hours, or if you experience bleeding between periods. Also seek medical attention if frequent periods cause significant fatigue, dizziness, or interfere with your daily activities, as these may indicate anemia or other complications.
How can I manage periods that come every 2 weeks during perimenopause?
Managing frequent periods involves tracking your cycles, maintaining adequate iron intake through diet or supplements, using appropriate menstrual products for heavier flows, and practicing stress-reduction techniques. Medical management options include hormonal contraceptives for cycle regulation, anti-inflammatory medications to reduce heavy bleeding, and iron supplementation to prevent anemia. Work with your healthcare provider to develop a personalized management plan.