Peroneal nerve pain can significantly impact your daily life, affecting how you walk, move, and perform routine activities. This important nerve, which runs down the leg and around the knee, plays a crucial role in controlling foot movement and sensation. Understanding its symptoms, causes, and treatment options is essential for anyone experiencing this condition.
Whether caused by injury, compression, or underlying medical conditions, peroneal nerve pain requires proper attention and care. This guide will help you understand the condition better and explore various management strategies to improve your quality of life.
Common Causes and Risk Factors
Peroneal nerve pain can develop from various circumstances and conditions:
- Direct trauma or injury to the knee area
- Prolonged pressure from crossing legs or sitting positions
- Knee surgery or hip replacement complications
- Diabetes and other metabolic disorders
- Prolonged bed rest or immobilization
- Sports injuries or repetitive movements
- Tight-fitting casts or braces
Athletes, individuals who frequently cross their legs, and those with certain medical conditions are at higher risk of developing peroneal nerve issues.
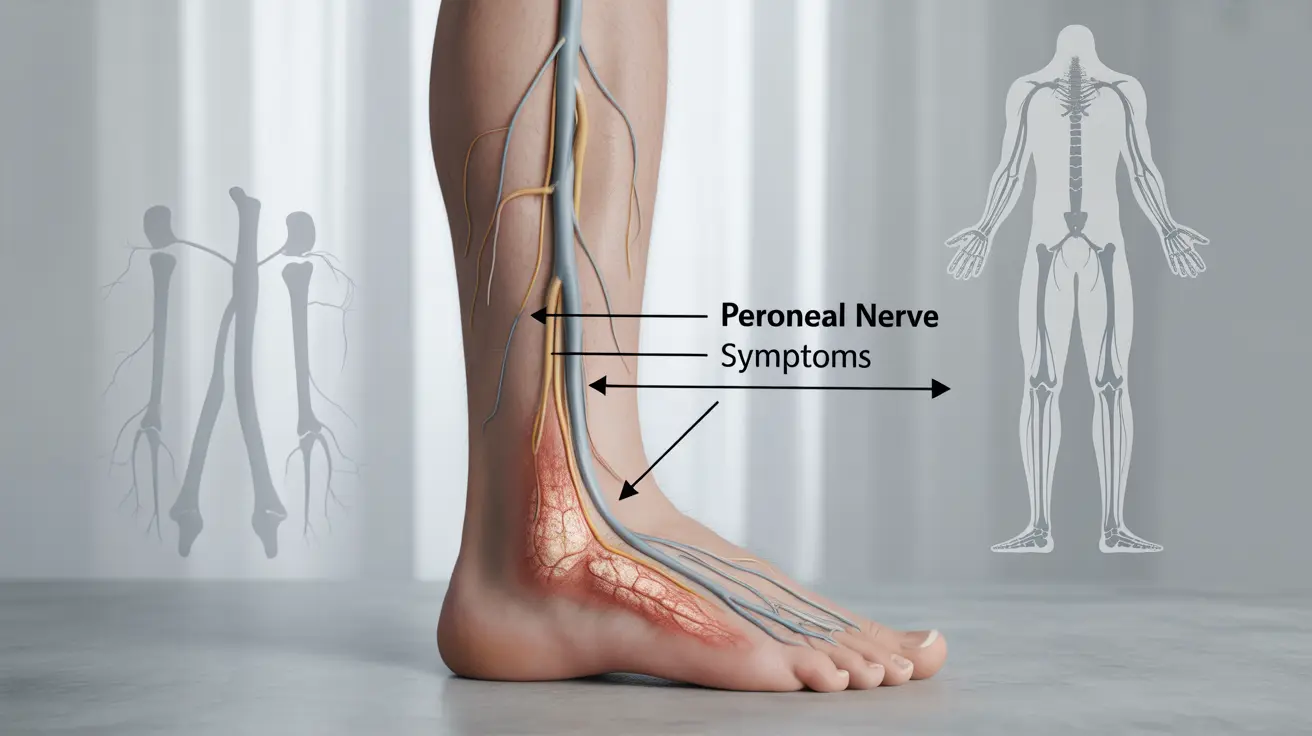
Recognizing the Symptoms
Early recognition of symptoms is crucial for proper treatment. Common signs include:
- Numbness or tingling in the top of the foot
- Weakness in foot muscles
- Difficulty lifting the foot (foot drop)
- Pain or burning sensation along the outer leg
- Decreased sensation in the outer leg and top of the foot
- Unstable walking pattern
Diagnostic Process
Healthcare providers use several methods to diagnose peroneal nerve problems:
Physical Examination
Your doctor will assess your walking pattern, muscle strength, and sensation in the affected area. They may also check for visible signs of injury or swelling.
Diagnostic Tests
Common diagnostic procedures include:
- Electromyography (EMG)
- Nerve conduction studies
- MRI scans
- X-rays to rule out other conditions
Treatment Approaches
Conservative Management
Initial treatment typically involves non-surgical methods:
- Physical therapy exercises
- Anti-inflammatory medications
- Supportive devices or braces
- Activity modification
- Proper footwear
Surgical Intervention
Surgery may be necessary in cases where:
- Conservative treatment fails
- There's severe nerve compression
- Significant trauma has occurred
- Tumors or cysts are present
Prevention and Self-Care
Several strategies can help prevent peroneal nerve problems:
- Avoid prolonged crossing of legs
- Use proper positioning during sleep and rest
- Maintain a healthy weight
- Wear properly fitting shoes and braces
- Practice regular stretching exercises
- Control underlying conditions like diabetes
Frequently Asked Questions
What are the common causes and risk factors of peroneal nerve pain?
Common causes include direct trauma, prolonged pressure from crossing legs, diabetes, surgery complications, and prolonged bed rest. Risk factors include certain occupations requiring repetitive movements, obesity, and underlying medical conditions.
What symptoms should make me suspect I have peroneal nerve injury or entrapment?
Key symptoms include foot drop (difficulty lifting the foot), numbness or tingling in the top of the foot, weakness in foot muscles, and pain or burning sensation along the outer leg.
How is peroneal nerve pain typically diagnosed by doctors?
Doctors use a combination of physical examination, EMG tests, nerve conduction studies, and imaging tests like MRI to diagnose peroneal nerve issues. They also review your medical history and symptoms.
What non-surgical and surgical treatment options are available for managing peroneal nerve pain?
Non-surgical options include physical therapy, anti-inflammatory medications, and supportive devices. Surgical options may include nerve decompression, nerve repair, or removal of tumors/cysts causing compression.
How can I prevent worsening of peroneal nerve pain or related complications like foot drop?
Prevention strategies include avoiding prolonged leg crossing, maintaining proper posture, using appropriate footwear, managing underlying conditions, and following prescribed exercise routines and treatment plans.