Placental abruption is a serious pregnancy complication that occurs when the placenta partially or completely separates from the inner wall of the uterus before delivery. This condition requires immediate medical attention as it can pose significant risks to both mother and baby. Understanding the different types of placental abruption and recognizing its symptoms early can make a crucial difference in outcomes.
Types of Placental Abruption
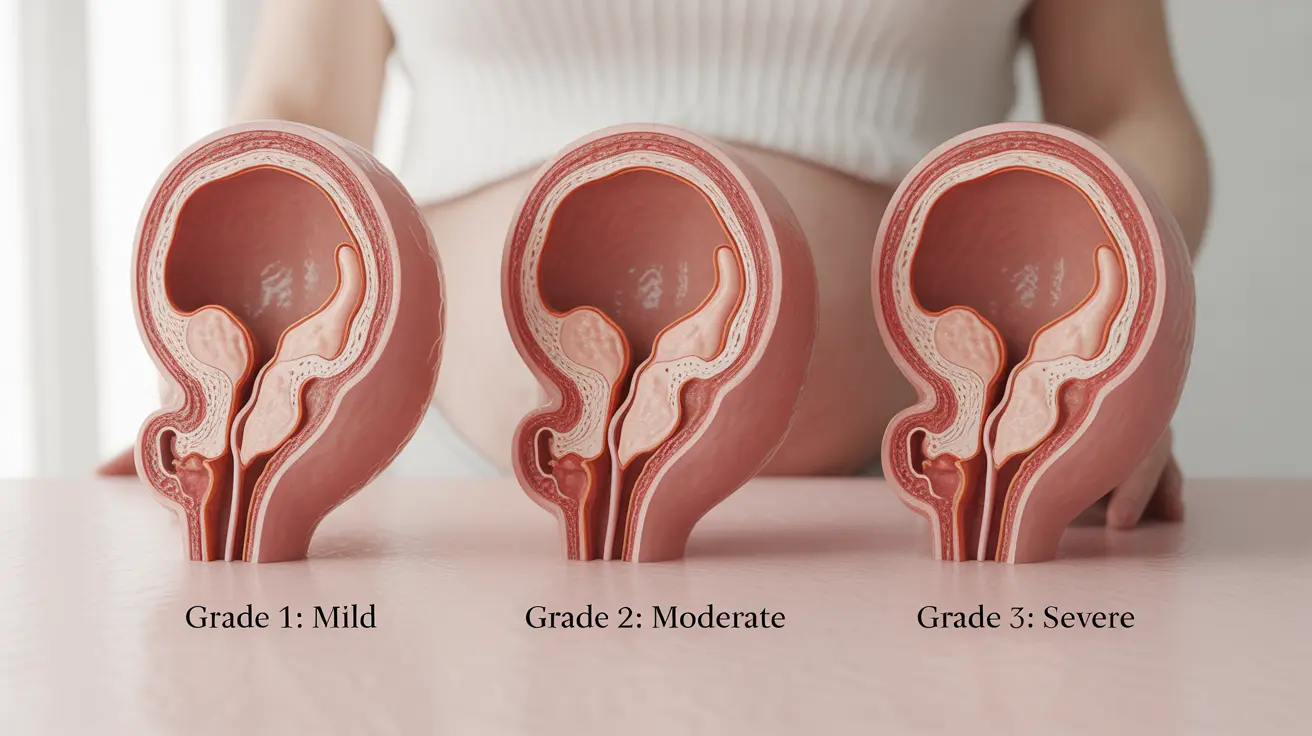
Medical professionals classify placental abruption into three distinct categories based on severity and symptoms:
Grade 1 (Mild) Abruption
This type involves separation of less than 25% of the placenta. Symptoms may be mild or absent, and many women continue their pregnancy with careful monitoring. The primary signs might include light vaginal bleeding and mild uterine tenderness.
Grade 2 (Moderate) Abruption
Affecting 25-50% of the placental surface, this type presents with moderate to heavy bleeding, significant uterine tenderness, and possible fetal distress. Close medical supervision is essential, and immediate hospitalization may be necessary.
Grade 3 (Severe) Abruption
This most serious form involves more than 50% of the placenta separating from the uterus. It typically requires emergency cesarean delivery due to the high risk to both mother and baby. Symptoms include severe bleeding, intense abdominal pain, and continuous uterine contractions.
Recognizing Warning Signs
Early detection of placental abruption is crucial for proper management. Key symptoms to watch for include:
- Vaginal bleeding (can be visible or concealed)
- Severe abdominal or back pain
- Uterine tenderness or rigidity
- Frequent contractions
- Decreased fetal movement
Diagnostic Approaches
Healthcare providers use several methods to diagnose placental abruption:
- Physical examination and symptom assessment
- Ultrasound imaging
- Fetal monitoring
- Blood tests to check for anemia or clotting issues
- Fibrinogen level testing
Treatment Strategies
Treatment depends on several factors, including:
- Gestational age
- Severity of the abruption
- Mother's condition
- Fetal status
In mild cases with a stable mother and baby, careful monitoring may be sufficient. However, severe cases often require immediate delivery, typically through emergency cesarean section.
Prevention and Risk Management
While not all cases can be prevented, certain measures can help reduce risk:
- Regular prenatal care
- Blood pressure management
- Avoiding tobacco, alcohol, and drugs
- Careful management of existing health conditions
- Proper treatment of any trauma or injury during pregnancy
Frequently Asked Questions
What are the different types of placental abruption and how do they affect pregnancy?
Placental abruption is classified into three grades: mild (Grade 1), moderate (Grade 2), and severe (Grade 3). Each grade represents different levels of placental separation and requires specific medical management approaches based on severity.
What symptoms should I watch for that might indicate placental abruption during pregnancy?
Key symptoms include vaginal bleeding, severe abdominal or back pain, uterine tenderness, frequent contractions, and decreased fetal movement. Any of these symptoms should prompt immediate medical attention.
How is placental abruption diagnosed and what tests are used to confirm it?
Diagnosis typically involves physical examination, ultrasound imaging, fetal monitoring, and blood tests. While ultrasound may not always show the abruption, it helps rule out other conditions and assess fetal well-being.
What are the treatment options for placental abruption based on its severity and type?
Treatment ranges from close monitoring for mild cases to immediate delivery for severe cases. The approach depends on factors such as gestational age, severity of separation, and the health status of both mother and baby.
What risks does placental abruption pose to the mother and baby, and how can complications be prevented?
Risks include maternal hemorrhage, preterm birth, and potential fetal distress or loss. Prevention focuses on regular prenatal care, managing risk factors, and avoiding known triggers like smoking and substance use.