Relapsing polychondritis can significantly impact the ears, causing both immediate discomfort and potential long-term complications. Understanding how this rare autoimmune condition affects ear cartilage is crucial for early recognition and proper management of symptoms.
This comprehensive guide explores the various ways relapsing polychondritis manifests in the ears, from initial inflammation to potential hearing complications, and discusses available treatment options to help manage these symptoms effectively.
Understanding Ear Involvement in Relapsing Polychondritis
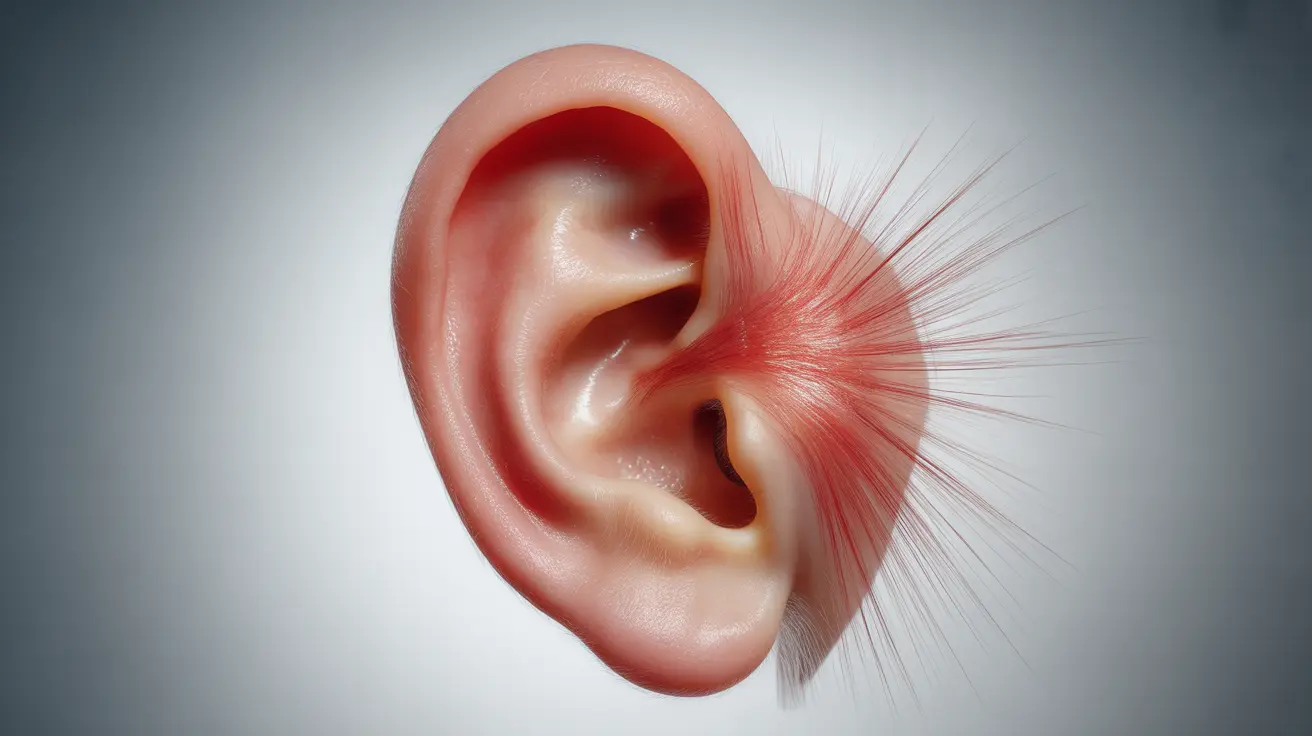
The ears are among the most commonly affected areas in relapsing polychondritis, with inflammation targeting the cartilage structures. This involvement can lead to noticeable physical changes and varying degrees of discomfort.
Early Signs and Symptoms
The initial symptoms of ear involvement typically include:
- Redness and swelling of the outer ear
- Tenderness and pain when touching the ear
- Warmth in the affected area
- Changes in ear shape or appearance
- Cartilage becoming soft or more flexible than normal
Characteristic Pattern of Inflammation
One distinctive feature of relapsing polychondritis is that the ear lobes remain unaffected during inflammation. This occurs because ear lobes don't contain cartilage, which is the primary target of the autoimmune response in this condition.
Long-term Effects and Complications
Without proper management, recurring episodes of ear inflammation can lead to several serious complications:
Structural Changes
Repeated inflammation can cause:
- Permanent ear deformity
- "Cauliflower ear" appearance
- Cartilage collapse
- Changes in ear flexibility and structure
Hearing and Balance Issues
Inner ear involvement may result in:
- Progressive hearing loss
- Tinnitus (ringing in the ears)
- Vertigo and balance problems
- Difficulty with spatial orientation
Treatment Approaches for Ear Symptoms
Medical Management
Treatment typically involves a multi-faceted approach:
- Anti-inflammatory medications
- Corticosteroids (both topical and systemic)
- Immunosuppressive drugs in severe cases
- Regular monitoring of hearing function
Protective Measures
Additional steps to prevent damage include:
- Avoiding trauma to the ears
- Protecting ears from extreme temperatures
- Regular medical follow-up
- Early intervention during flare-ups
Frequently Asked Questions
What are the common ear symptoms of relapsing polychondritis and how can I recognize them early?
Early ear symptoms include redness, swelling, and pain in the outer ear cartilage. The ear may feel warm to touch and become increasingly tender. Unlike typical ear infections, the inflammation specifically affects the cartilage portions of the ear, leaving the earlobes unaffected.
How does relapsing polychondritis affect the ears long-term, and what are the risks of hearing loss?
Long-term effects can include permanent ear deformity, cartilage collapse, and progressive hearing loss. Repeated inflammation episodes can damage both the outer ear structure and inner ear components, potentially leading to permanent hearing impairment.
What treatment options are available to reduce ear inflammation and prevent damage in relapsing polychondritis?
Treatment typically includes anti-inflammatory medications, corticosteroids, and sometimes immunosuppressive drugs. Early intervention during flares is crucial to prevent permanent damage. Regular monitoring and protective measures are also important components of management.
Why do the ear lobes usually remain unaffected in relapsing polychondritis ear inflammation?
Ear lobes remain unaffected because they don't contain cartilage, which is the primary target of the autoimmune response in relapsing polychondritis. The condition specifically attacks cartilage tissue, leaving cartilage-free areas like the ear lobes unchanged.
Can relapsing polychondritis cause balance problems or vertigo due to inner ear involvement?
Yes, relapsing polychondritis can affect the inner ear structures, leading to balance problems and vertigo. When inflammation impacts the vestibular system, patients may experience dizziness, difficulty with spatial orientation, and problems maintaining balance.