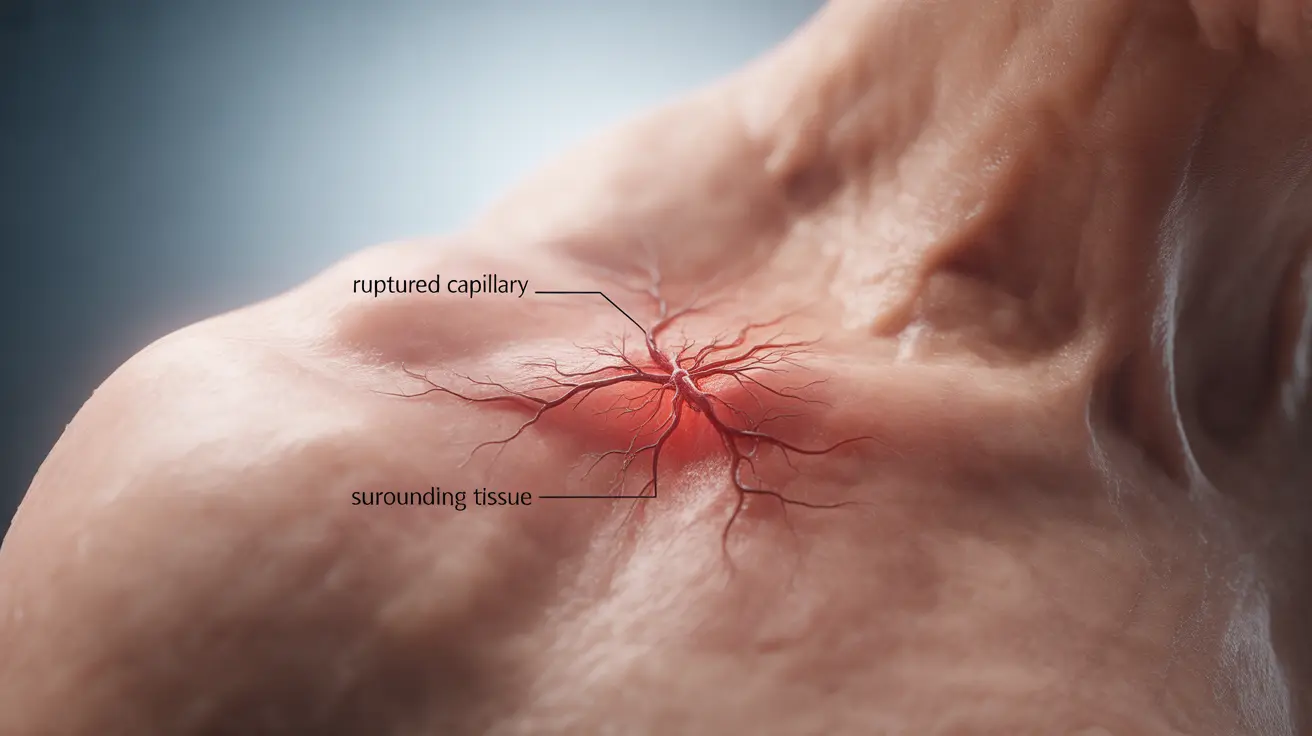
When a blood vessel bursts beneath your skin, it can be both alarming and uncomfortable. These popped blood vessels, also known as broken capillaries or petechiae, are relatively common occurrences that can happen to anyone. Understanding their causes, knowing when to seek medical attention, and learning about treatment options can help you manage this condition effectively.
What Causes Blood Vessels to Pop Under the Skin?
Blood vessels can burst for various reasons, ranging from minor trauma to underlying health conditions. Common causes include:
- Physical injury or trauma
- Sudden pressure changes
- Straining during physical activities
- Violent coughing or sneezing
- Heavy lifting
- Prolonged sun exposure
- Aging and weakening vessel walls
In some cases, everyday activities that increase pressure in your blood vessels can lead to their rupture, especially if the vessels are already weakened or compromised.
Identifying When Medical Attention Is Needed
While most popped blood vessels heal naturally over time, certain signs indicate the need for medical evaluation:
Warning Signs
- Large areas of discoloration
- Severe pain or swelling
- Frequent or recurring incidents
- Accompanying symptoms like dizziness
- No improvement after several weeks
If you experience any of these symptoms, it's important to consult a healthcare provider for proper assessment and treatment.
Effective At-Home Treatment Methods
Many cases of popped blood vessels can be managed effectively at home using these approaches:
Immediate Care
- Apply cold compresses
- Elevate the affected area
- Rest and avoid strenuous activity
- Protect the area from further injury
Long-Term Care
- Use gentle skincare products
- Maintain good circulation
- Stay hydrated
- Protect skin from sun damage
Risk Factors and Prevention
Several factors can increase your risk of experiencing popped blood vessels:
Medical Conditions
- High blood pressure
- Blood clotting disorders
- Diabetes
- Liver disease
- Vitamin K deficiency
Medications
Certain medications can increase the likelihood of blood vessel rupture, including:
- Blood thinners
- Aspirin and NSAIDs
- Steroids
- Some dietary supplements
Professional Treatment Options
For persistent or cosmetically concerning cases, especially on the face, several medical treatments are available:
- Laser therapy
- Sclerotherapy
- Intense Pulsed Light (IPL) treatment
- Topical medications
- Chemical peels
Frequently Asked Questions
What causes a popped blood vessel under the skin and how can everyday actions like coughing or sneezing lead to it? Popped blood vessels occur when increased pressure causes small capillaries to burst. Actions like coughing or sneezing create sudden pressure changes in your body, which can strain and rupture weakened blood vessels, especially in sensitive areas.
How can I tell if a popped blood vessel needs medical attention or will heal on its own? Most popped blood vessels heal naturally within 2-3 weeks. Seek medical attention if you experience severe pain, large areas of discoloration, frequent occurrences, or if the area doesn't improve after several weeks.
What are the most effective at-home treatments for a popped blood vessel in the hand or face? Apply cold compresses immediately, elevate the affected area, and avoid touching or rubbing the spot. For facial vessels, use gentle skincare products and protect the area from sun exposure. On hands, minimize movement and protect the area from further injury.
Can certain medications or health conditions increase the risk of blood vessels bursting under the skin? Yes, blood thinners, NSAIDs, and conditions like high blood pressure, diabetes, and blood disorders can increase your risk. Some vitamin deficiencies and liver conditions may also make blood vessels more prone to breaking.
What are the available medical treatments to reduce visible broken blood vessels on the face? Professional treatments include laser therapy, sclerotherapy, and IPL treatments. These procedures can effectively reduce the appearance of broken blood vessels, though multiple sessions may be needed for optimal results.