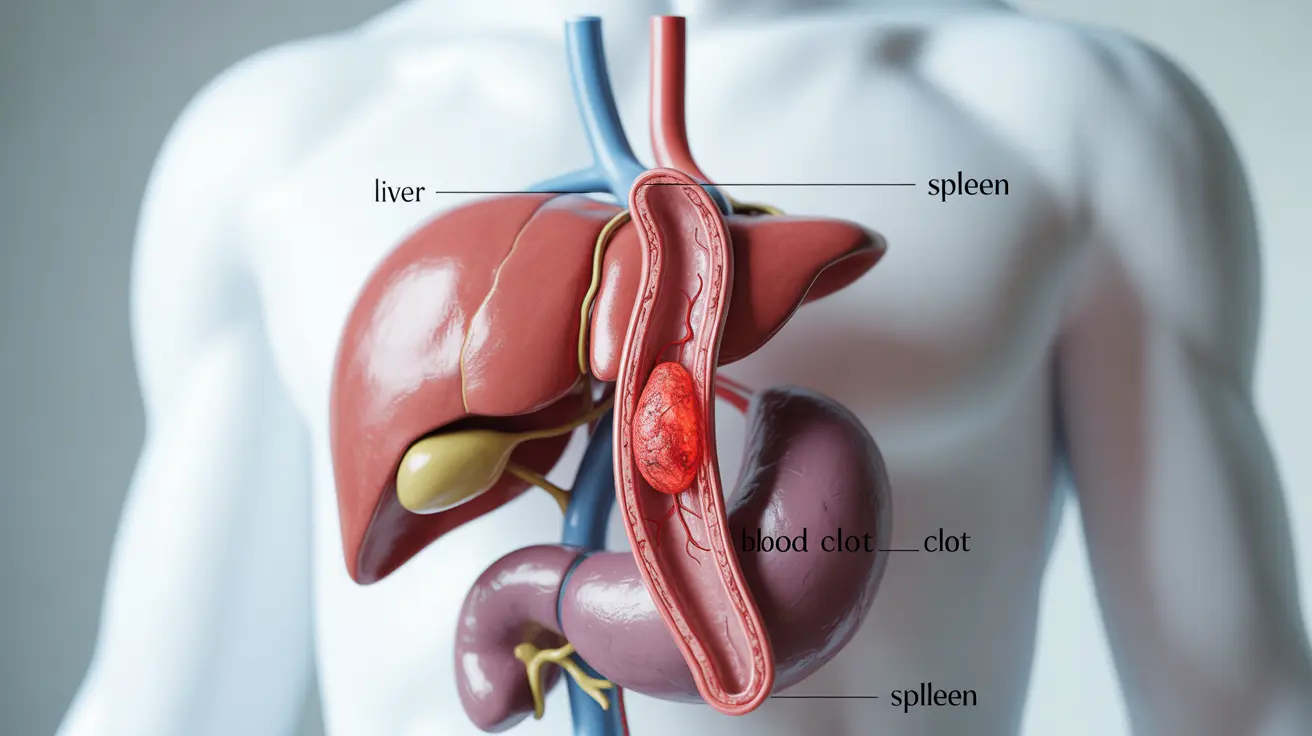
Portal vein thrombosis is a serious medical condition that occurs when a blood clot forms in the portal vein, the main blood vessel that carries blood from the digestive organs to the liver. This condition can significantly impact liver function and overall health, making early detection and proper management crucial for optimal outcomes.
Understanding the symptoms, causes, and treatment options for portal vein thrombosis is essential for both healthcare providers and patients. This comprehensive guide explores the key aspects of this condition and provides valuable insights into its management.
Understanding Portal Vein Thrombosis
Portal vein thrombosis develops when blood clots block or restrict blood flow through the portal vein system. This blockage can occur suddenly (acute) or develop gradually (chronic), each presenting with different symptoms and requiring specific approaches to treatment.
Common Signs and Symptoms
The symptoms of portal vein thrombosis can vary significantly among individuals, but may include:
- Abdominal pain, particularly in the upper right portion
- Nausea and vomiting
- Loss of appetite
- Enlarged spleen
- Portal hypertension
- Ascites (fluid accumulation in the abdomen)
- Fever in some cases
Risk Factors and Causes
Several underlying conditions and circumstances can increase the risk of developing portal vein thrombosis:
Medical Conditions
- Cirrhosis of the liver
- Blood clotting disorders
- Inflammatory bowel disease
- Pancreatitis
- Abdominal infections
Other Risk Factors
- Recent abdominal surgery
- Cancer, particularly liver cancer
- Pregnancy
- Use of oral contraceptives
- Obesity
Diagnosis and Assessment
Accurate diagnosis of portal vein thrombosis requires a combination of clinical evaluation and specialized imaging techniques. Healthcare providers typically employ several diagnostic tools:
Imaging Studies
- Doppler ultrasound
- CT scan with contrast
- MRI/MRV
- Angiography in select cases
Laboratory Tests
- Complete blood count
- Liver function tests
- Coagulation profile
- Thrombophilia testing when indicated
Treatment Approaches
The treatment strategy for portal vein thrombosis depends on various factors, including the timing of diagnosis, extent of thrombosis, and underlying conditions. Common treatment approaches include:
Medical Management
- Anticoagulation therapy
- Management of underlying conditions
- Prevention of complications
- Regular monitoring of liver function
Surgical Interventions
In severe cases or when medical management proves insufficient, surgical procedures may be necessary. These might include thrombectomy or placement of transjugular intrahepatic portosystemic shunts (TIPS).
Prevention and Long-term Management
Preventing complications and managing long-term health outcomes requires a comprehensive approach:
- Regular medical follow-up
- Lifestyle modifications
- Management of underlying conditions
- Medication compliance
- Regular monitoring of liver health
Frequently Asked Questions
What are the common symptoms and warning signs of portal vein thrombosis?
Common symptoms include abdominal pain (especially in the upper right area), nausea, vomiting, loss of appetite, and in some cases, the development of ascites. Some patients may also experience fever and an enlarged spleen.
What causes portal vein thrombosis and who is at risk for developing it?
Portal vein thrombosis can be caused by various factors, including liver cirrhosis, blood clotting disorders, inflammatory conditions, and cancer. People with recent abdominal surgery, pregnancy, or those using oral contraceptives may have an increased risk.
How is portal vein thrombosis diagnosed through imaging and laboratory tests?
Diagnosis typically involves imaging studies such as Doppler ultrasound, CT scans with contrast, or MRI/MRV. Laboratory tests, including blood counts, liver function tests, and coagulation studies, are also performed to assess the condition and identify underlying causes.
What treatment options are available for managing portal vein thrombosis?
Treatment options include anticoagulation therapy, management of underlying conditions, and in some cases, surgical interventions like thrombectomy or TIPS. The specific treatment approach depends on factors such as the timing of diagnosis and severity of the condition.
What complications can arise from untreated portal vein thrombosis and how can they be prevented?
Untreated portal vein thrombosis can lead to serious complications including portal hypertension, esophageal varices, and liver damage. Prevention involves regular medical monitoring, proper management of underlying conditions, and adherence to prescribed treatments.