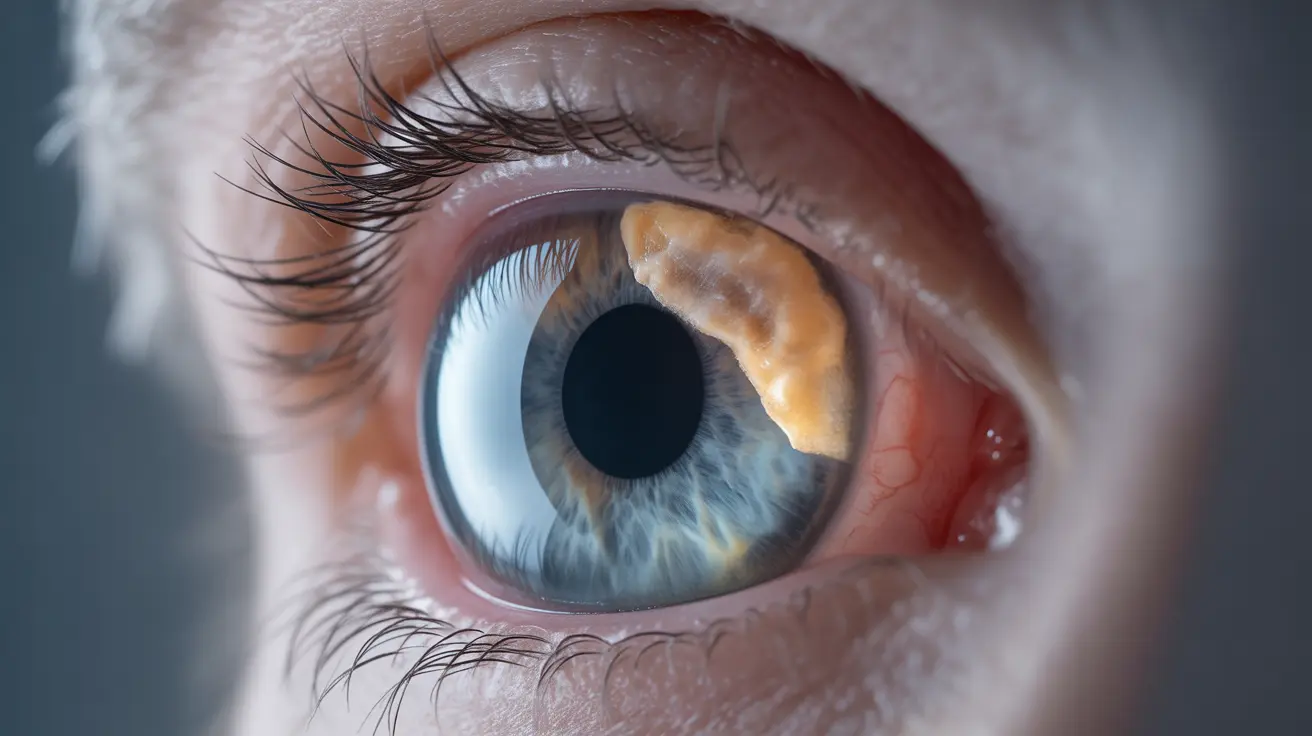
A posterior subcapsular cataract (PSC) is a specific type of eye condition that develops at the back of the lens, directly in front of the lens capsule. This unique form of cataract can significantly impact vision and often progresses more rapidly than other types of cataracts. Understanding its symptoms, causes, and treatment options is crucial for early detection and successful management.
Unlike other forms of cataracts that typically develop slowly with age, posterior subcapsular cataracts can affect younger individuals and may progress more quickly, making prompt medical attention particularly important.
Key Symptoms and Recognition
Posterior subcapsular cataracts present with distinct characteristics that set them apart from other types of cataracts. Common symptoms include:
- Disproportionate difficulty seeing in bright light
- Significantly reduced near vision
- Improved vision in dimmer conditions
- Rapidly declining visual clarity
- Particular difficulty with reading
These symptoms can develop relatively quickly, sometimes over months rather than the years typically associated with age-related cataracts.
Risk Factors and Causes
Several factors can contribute to the development of posterior subcapsular cataracts:
- Long-term steroid medication use
- Diabetes
- Severe myopia (nearsightedness)
- Previous eye trauma or inflammation
- Exposure to radiation
- Genetic predisposition
Understanding these risk factors is essential for both prevention and early intervention strategies.
Progression and Development
Posterior subcapsular cataracts typically progress more rapidly than nuclear or cortical cataracts. The speed of progression can vary significantly among individuals, but many patients report noticeable vision changes within months of onset. This faster progression rate often necessitates more urgent medical attention and treatment planning.
Treatment Approaches
The primary treatment for posterior subcapsular cataracts is surgical intervention. Modern cataract surgery is highly effective and typically involves:
- Removal of the clouded lens
- Replacement with an artificial intraocular lens
- Minimally invasive techniques
- Quick recovery time
- High success rates
The decision to undergo surgery often depends on how significantly the cataract affects daily activities and quality of life.
Prevention Strategies
While not all cases of posterior subcapsular cataracts can be prevented, several measures may help reduce risk:
- Regular eye examinations
- Careful management of underlying conditions like diabetes
- Protection from UV radiation
- Maintaining a healthy lifestyle
- Discussing steroid use with healthcare providers
Frequently Asked Questions
What are the common symptoms of a posterior subcapsular cataract?
Common symptoms include decreased near vision, particular sensitivity to bright light, improved vision in dimmer conditions, and relatively rapid vision deterioration. Reading and close-up work often become especially challenging.
What causes posterior subcapsular cataracts and who is at risk of developing them?
Primary causes include prolonged steroid use, diabetes, eye trauma, and radiation exposure. People at higher risk include those on long-term steroid medication, diabetics, individuals with previous eye injuries, and those with certain genetic predispositions.
How fast do posterior subcapsular cataracts progress compared to other types?
Posterior subcapsular cataracts typically progress more rapidly than other cataract types, often showing significant vision changes within months rather than the years usually associated with age-related cataracts.
What treatment options are available for posterior subcapsular cataracts and how effective is surgery?
The primary treatment is surgical removal of the clouded lens and replacement with an artificial intraocular lens. Modern cataract surgery is highly effective, with success rates exceeding 98% and typically results in significant vision improvement.
How can I reduce my risk of developing a posterior subcapsular cataract?
Risk reduction strategies include maintaining regular eye check-ups, managing underlying health conditions, protecting eyes from UV radiation, maintaining a healthy lifestyle, and discussing any long-term steroid use with healthcare providers.