While pregnancy and childbirth are often viewed as natural processes, they can sometimes lead to serious cardiovascular complications that many new mothers aren't aware of. A postpartum heart attack, though relatively rare, represents a life-threatening medical emergency that can occur during the first few months after delivery.
Understanding the unique characteristics of postpartum heart attacks is crucial for new mothers, their families, and healthcare providers. Unlike heart attacks in the general population, these cardiac events often present with distinct symptoms and underlying causes that require specialized recognition and treatment approaches.
Recognizing the Warning Signs of Postpartum Heart Attack
The symptoms of a postpartum heart attack can be particularly challenging to identify because they may overlap with normal postpartum recovery experiences. New mothers often attribute chest discomfort, shortness of breath, or fatigue to the physical demands of childbirth and caring for a newborn.
Classic heart attack symptoms in postpartum women include severe chest pain or pressure that may radiate to the arms, neck, jaw, or back. However, women experiencing postpartum heart attacks may also present with less typical symptoms such as nausea, vomiting, excessive sweating, dizziness, or overwhelming fatigue that goes beyond normal postpartum tiredness.
What makes postpartum heart attack symptoms particularly concerning is their potential to be dismissed as normal recovery-related discomfort. Unlike typical heart attacks that often occur during physical exertion, postpartum heart attacks can strike suddenly during rest or routine activities, making recognition even more critical.
Understanding the Underlying Causes
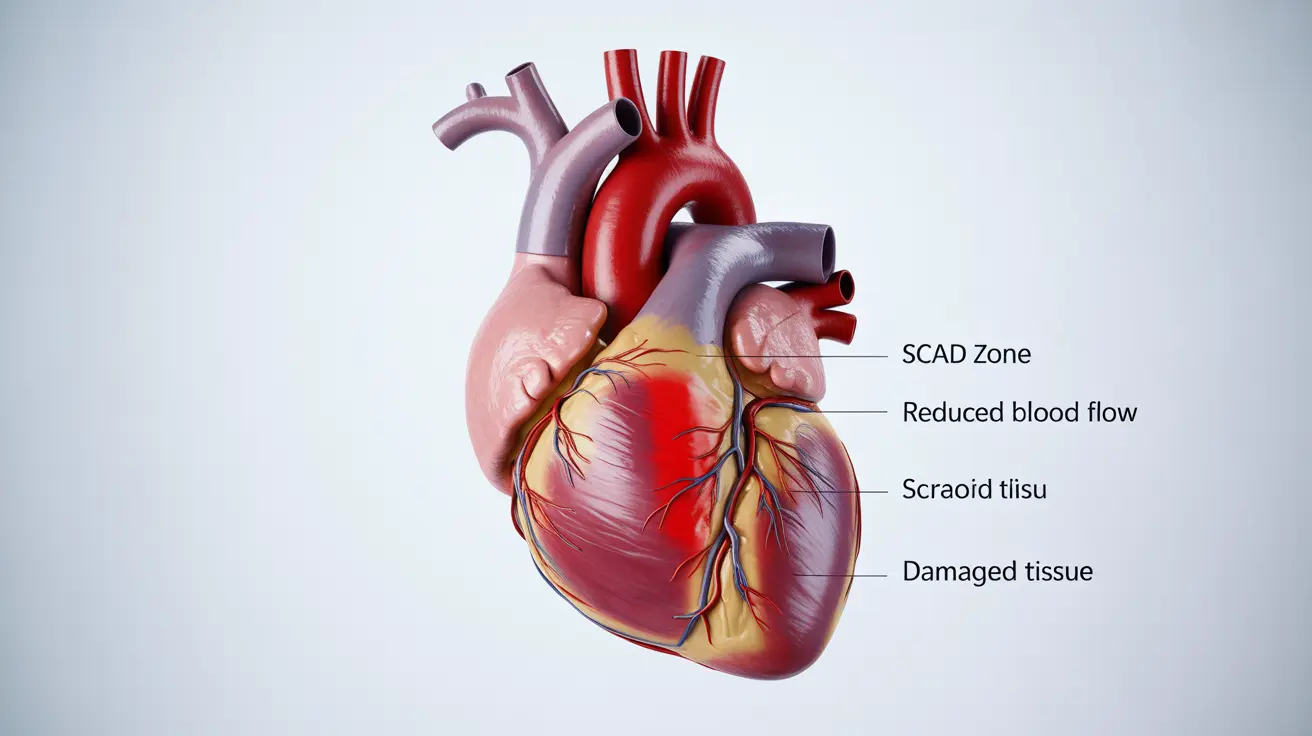
The primary cause of postpartum heart attacks differs significantly from heart attacks in other populations. Spontaneous coronary artery dissection (SCAD) accounts for approximately 80% of postpartum heart attacks, making it the leading cause of cardiac events in this population.
SCAD occurs when the inner wall of a coronary artery tears spontaneously, creating a false channel that can block blood flow to the heart muscle. The hormonal changes during pregnancy and the postpartum period, particularly fluctuating estrogen levels, are believed to contribute to arterial wall weakness that predisposes women to this condition.
Other contributing factors include the significant hemodynamic changes that occur during pregnancy, increased blood volume, elevated blood pressure during labor and delivery, and the physical stress of childbirth. Peripartum cardiomyopathy, a condition where the heart muscle weakens during late pregnancy or early postpartum, can also increase the risk of cardiovascular complications.
Diagnostic Procedures and Testing
Diagnosing a postpartum heart attack requires prompt medical evaluation and specialized testing. Healthcare providers typically begin with a thorough physical examination and medical history, paying particular attention to pregnancy and delivery complications.
An electrocardiogram (ECG) is usually the first diagnostic test performed to detect abnormal heart rhythms or signs of heart muscle damage. Blood tests measuring cardiac enzymes, particularly troponin levels, can confirm heart muscle damage and help determine the severity of the cardiac event.
Advanced imaging techniques play a crucial role in postpartum heart attack diagnosis. Echocardiography can assess heart function and detect wall motion abnormalities. Cardiac catheterization, while sometimes necessary, requires careful consideration in breastfeeding mothers due to contrast agent exposure. Coronary CT angiography or cardiac MRI may be preferred alternatives in certain situations.
Treatment Approaches and Considerations
Treatment for postpartum heart attacks requires specialized approaches that consider both the mother's immediate cardiac needs and potential impacts on breastfeeding. The management strategy often depends on whether SCAD or other causes are responsible for the cardiac event.
For SCAD-related postpartum heart attacks, conservative medical management is often preferred over invasive procedures. This approach typically includes antiplatelet therapy, beta-blockers, and ACE inhibitors, with careful consideration of medication safety during breastfeeding.
When interventional procedures are necessary, percutaneous coronary intervention (PCI) may be performed, though it carries additional risks in SCAD cases due to the potential for extending the dissection. In severe cases, coronary artery bypass surgery might be required.
Medication selection requires careful evaluation of safety profiles during breastfeeding. Many cardiac medications can be safely used while nursing, but dosing and timing may need adjustment to minimize infant exposure.
Risk Factors and Prevention Strategies
Several risk factors increase the likelihood of experiencing a postpartum heart attack. Advanced maternal age, particularly over 35 years, significantly elevates risk. Multiple pregnancies, pregnancy-related hypertensive disorders like preeclampsia, and gestational diabetes also contribute to increased cardiovascular risk.
Pre-existing cardiovascular conditions, family history of heart disease, smoking, and obesity further compound the risk. Women who have experienced pregnancy complications such as placental abruption or postpartum hemorrhage may also face elevated cardiac risks.
Prevention strategies focus on optimizing cardiovascular health before, during, and after pregnancy. This includes maintaining a healthy weight, following a heart-healthy diet rich in fruits, vegetables, and whole grains, and engaging in appropriate physical activity as recommended by healthcare providers.
Regular prenatal care with monitoring of blood pressure, blood sugar, and other cardiovascular risk factors is essential. Postpartum follow-up should include cardiovascular assessment, particularly for women who experienced pregnancy complications.
Long-term Outlook and Recovery
The prognosis for women who survive a postpartum heart attack varies depending on the extent of heart muscle damage and underlying causes. Many women can achieve good long-term outcomes with appropriate treatment and lifestyle modifications.
Cardiac rehabilitation programs can play a vital role in recovery, helping new mothers safely return to physical activity while managing their cardiac condition. These programs also provide education about heart-healthy lifestyle choices and ongoing risk management.
Future pregnancy considerations require careful counseling and planning with maternal-fetal medicine specialists and cardiologists. While some women can safely have additional pregnancies, others may face increased risks that require specialized monitoring and care.
Frequently Asked Questions
What are the common symptoms of a postpartum heart attack and how do they differ from typical heart attack symptoms?
Postpartum heart attack symptoms include severe chest pain, shortness of breath, nausea, excessive sweating, and overwhelming fatigue. These symptoms can be easily mistaken for normal postpartum recovery discomfort, making them particularly dangerous. Unlike typical heart attacks that often occur during exertion, postpartum heart attacks can happen suddenly during rest or routine activities, and the chest pain may be less pronounced while other symptoms like nausea and fatigue are more prominent.
What causes a postpartum heart attack, and why is spontaneous coronary artery dissection (SCAD) a major factor?
Spontaneous coronary artery dissection (SCAD) causes approximately 80% of postpartum heart attacks. SCAD occurs when the coronary artery wall tears spontaneously, creating a blockage that prevents blood flow to the heart muscle. The hormonal changes during pregnancy and postpartum, particularly fluctuating estrogen levels, weaken arterial walls and increase susceptibility to this condition. The physical stress of childbirth and hemodynamic changes during pregnancy also contribute to the risk.
How is a postpartum heart attack diagnosed and what tests are usually performed?
Diagnosis typically begins with a physical examination and medical history review. An electrocardiogram (ECG) is performed first to detect heart rhythm abnormalities, followed by blood tests measuring cardiac enzymes like troponin to confirm heart muscle damage. Advanced imaging may include echocardiography to assess heart function, and in some cases, coronary CT angiography or cardiac MRI. Cardiac catheterization may be necessary but requires careful consideration in breastfeeding mothers due to contrast agent exposure.
What treatments are available for postpartum heart attacks, and how do they differ from treatments for other heart attacks?
Treatment for postpartum heart attacks often involves conservative medical management, especially when SCAD is the cause. This includes antiplatelet therapy, beta-blockers, and ACE inhibitors, with careful consideration of breastfeeding safety. Unlike other heart attacks where aggressive intervention is common, SCAD-related postpartum heart attacks may be managed without invasive procedures since intervention can potentially worsen the dissection. When procedures are necessary, percutaneous coronary intervention or bypass surgery may be performed with specialized considerations for new mothers.
What risk factors increase the chance of having a postpartum heart attack and how can women reduce their risk?
Risk factors include advanced maternal age (over 35), multiple pregnancies, preeclampsia, gestational diabetes, pre-existing heart conditions, family history of heart disease, smoking, and obesity. Women can reduce their risk by maintaining a healthy weight, following a heart-healthy diet, staying physically active as recommended by their healthcare provider, receiving regular prenatal care with cardiovascular monitoring, managing pregnancy complications promptly, and attending postpartum follow-up appointments that include cardiovascular assessment.