When navigating hormone therapy options or understanding reproductive health, two terms frequently arise that sound remarkably similar but represent distinct substances: progestin and progesterone. While these hormones share some similarities in function, understanding the differences between progestin vs progesterone is crucial for making informed healthcare decisions.
Both substances play vital roles in women's health, particularly in regulating menstrual cycles, supporting pregnancy, and serving as components in hormone replacement therapy. However, their origins, chemical structures, and effects on the body can vary significantly, influencing treatment outcomes and potential side effects.
Understanding Progesterone: The Body's Natural Hormone
Progesterone is a naturally occurring hormone produced primarily by the ovaries during the second half of the menstrual cycle. This bioidentical hormone plays essential roles in preparing the uterine lining for potential pregnancy and maintaining early pregnancy if conception occurs.
The body produces progesterone through a complex process involving the corpus luteum, which forms after ovulation. During pregnancy, the placenta takes over progesterone production, maintaining levels necessary for fetal development and preventing additional ovulation.
Natural progesterone serves multiple functions beyond reproduction, including supporting bone density, promoting healthy sleep patterns, and helping regulate mood. Its molecular structure is identical to what the body produces naturally, which often translates to better compatibility and fewer adverse reactions.
What Is Progestin: Synthetic Hormone Alternatives
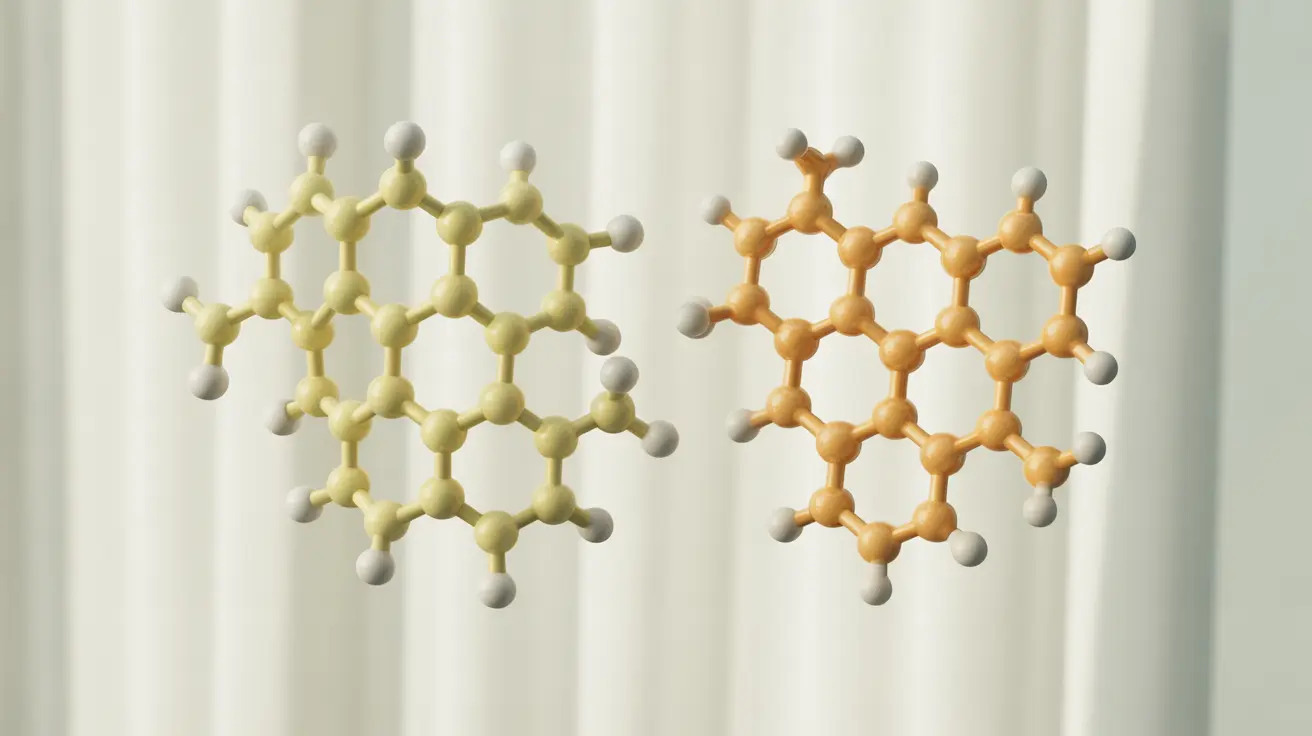
Progestin refers to synthetic compounds designed to mimic progesterone's effects in the body. These laboratory-created substances share similar functions with natural progesterone but possess different chemical structures that can influence how the body processes and responds to them.
Various types of progestins exist, each with unique characteristics and applications. Common examples include medroxyprogesterone acetate, levonorgestrel, and norethindrone. These synthetic alternatives were developed to provide more stable, long-lasting effects and improved oral bioavailability compared to natural progesterone.
Progestins are widely used in birth control pills, hormone replacement therapy, and various gynecological treatments. Their synthetic nature allows for precise dosing and extended shelf life, making them practical choices for pharmaceutical applications.
Medical Applications and Treatment Uses
Both progesterone and progestins serve important roles in modern medicine, though their specific applications may differ based on individual patient needs and treatment goals.
Natural Progesterone Uses
Bioidentical progesterone is commonly prescribed for hormone replacement therapy, particularly for women experiencing perimenopause or menopause. It's also used to support fertility treatments, manage irregular menstrual cycles, and address progesterone deficiency conditions.
Many healthcare providers prefer natural progesterone for patients seeking bioidentical hormone therapy, as its molecular structure matches what the body naturally produces. This similarity often results in more predictable responses and potentially fewer side effects.
Progestin Applications
Synthetic progestins are frequently used in contraceptive methods, including birth control pills, intrauterine devices (IUDs), and injectable contraceptives. They're also components in certain hormone replacement therapy formulations, particularly when combined with estrogen.
Progestins offer advantages in terms of dosing consistency and manufacturing stability, making them suitable for mass-produced pharmaceutical products. Their varied formulations allow healthcare providers to select specific types based on individual patient requirements.
Safety Considerations and Health Risks
When comparing safety profiles, both progesterone and progestins carry potential risks and benefits that must be carefully evaluated for each individual patient.
Natural progesterone generally demonstrates a more favorable safety profile, with fewer reported adverse effects and lower risks of certain complications. Research suggests that bioidentical progesterone may pose less risk for blood clots, cardiovascular events, and certain cancers compared to some synthetic alternatives.
Progestins, while effective for their intended uses, may carry increased risks for certain health conditions. Some studies have associated specific progestins with higher rates of blood clots, mood changes, and cardiovascular complications, though individual responses vary significantly.
The choice between progesterone and progestin should always be made in consultation with healthcare providers who can assess individual risk factors, medical history, and treatment objectives to determine the most appropriate option.
Side Effects and Body Response Differences
The body's response to progesterone versus progestins can differ substantially, influencing both therapeutic effectiveness and side effect profiles.
Common side effects of natural progesterone may include mild drowsiness, breast tenderness, and occasional mood fluctuations. However, these effects are often less severe and more transient compared to synthetic alternatives, as the body recognizes and processes the hormone more naturally.
Progestins may produce more pronounced side effects, including significant mood changes, weight gain, irregular bleeding patterns, and potential impacts on cholesterol levels. The specific side effect profile depends on the type of progestin used and individual patient factors.
Understanding these differences helps patients and healthcare providers make informed decisions about hormone therapy options, weighing potential benefits against possible adverse effects for each individual situation.
Frequently Asked Questions
What is the difference between progestin and progesterone hormones?
The primary difference lies in their origin and chemical structure. Progesterone is a naturally occurring hormone produced by the ovaries, while progestin refers to synthetic compounds created in laboratories to mimic progesterone's effects. Natural progesterone has an identical molecular structure to what the body produces, whereas progestins have modified chemical structures that can affect how the body processes them.
How do the side effects of progestin compare to natural progesterone?
Natural progesterone typically causes fewer and milder side effects compared to synthetic progestins. Progesterone side effects may include mild drowsiness, breast tenderness, and occasional mood changes. Progestins often produce more pronounced effects, including significant mood swings, weight gain, irregular bleeding, and potential cholesterol level changes. The severity and type of side effects can vary based on the specific progestin formulation used.
Which hormone is safer to use in hormone replacement therapy: progestin or progesterone?
Research generally suggests that natural progesterone may be safer for hormone replacement therapy. Studies indicate that bioidentical progesterone may pose lower risks for blood clots, cardiovascular events, and certain cancers compared to some synthetic progestins. However, individual safety depends on personal health factors, medical history, and specific treatment needs, making consultation with healthcare providers essential for determining the most appropriate option.
What are the common medical uses of progesterone versus progestin?
Natural progesterone is commonly used in bioidentical hormone replacement therapy, fertility treatments, menstrual cycle regulation, and addressing progesterone deficiency. Progestins are frequently used in contraceptive methods including birth control pills, IUDs, and injectable contraceptives, as well as in certain hormone replacement therapy formulations. The choice depends on specific medical needs, treatment goals, and individual patient factors.
Can progestin and progesterone affect breast cancer risk differently?
Current research suggests potential differences in breast cancer risk between progesterone and progestins. Some studies indicate that natural progesterone may pose lower breast cancer risks compared to certain synthetic progestins, particularly when used in hormone replacement therapy. However, both hormones can influence breast tissue, and individual risk assessment should always involve comprehensive evaluation by oncologists or specialized healthcare providers, considering personal and family medical history.