Type 2 diabetes is a chronic condition that naturally evolves over time, affecting millions of Americans each year. Understanding how this condition progresses is crucial for both patients and healthcare providers to manage it effectively and prevent serious complications.
This comprehensive guide explores the various stages of type 2 diabetes progression, from early insulin resistance to potential complications, and provides valuable insights into managing this condition effectively over time.
The Natural Course of Type 2 Diabetes
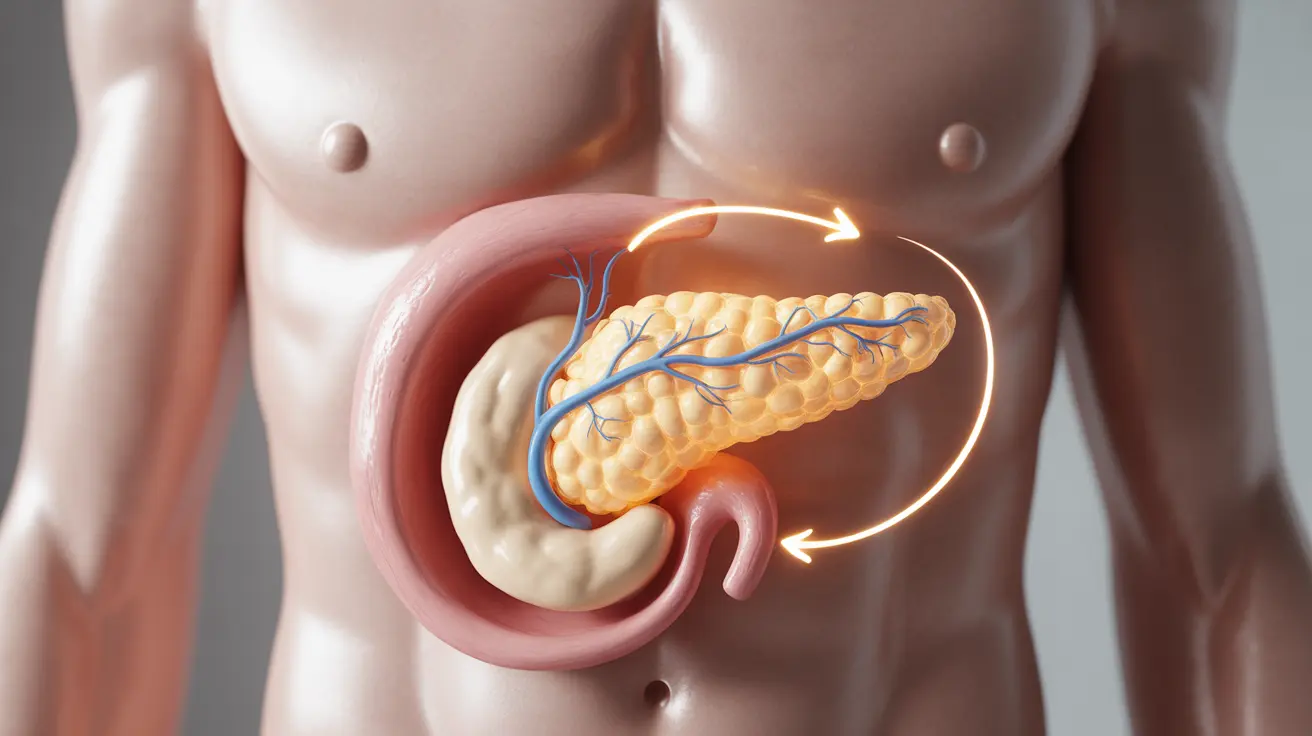
Type 2 diabetes typically develops gradually, beginning with insulin resistance in the body's cells. As the condition progresses, the pancreas struggles to produce enough insulin to overcome this resistance, leading to elevated blood sugar levels and worsening symptoms over time.
Understanding Insulin Resistance
Insulin resistance occurs when cells become less responsive to insulin, the hormone responsible for helping glucose enter cells for energy. As this resistance increases, the pancreas must work harder to produce more insulin, eventually leading to pancreatic beta cell dysfunction and decreased insulin production.
Key Factors Affecting Disease Progression
Lifestyle Influences
Several lifestyle factors can significantly impact the rate at which type 2 diabetes progresses:
- Diet and nutrition choices
- Physical activity levels
- Stress management
- Sleep quality
- Weight management
Genetic and Environmental Factors
Various genetic and environmental elements can influence how quickly the condition advances:
- Family history of diabetes
- Age and ethnicity
- Environmental toxins
- Chronic inflammation
- Concurrent health conditions
Monitoring Disease Progression
Blood Sugar Testing
Regular blood sugar monitoring is essential for tracking disease progression and maintaining optimal control:
- Daily blood glucose checks
- Quarterly A1C tests
- Continuous glucose monitoring when appropriate
Other Important Health Markers
Healthcare providers typically monitor several additional factors to assess disease progression:
- Blood pressure readings
- Cholesterol levels
- Kidney function tests
- Eye examinations
- Foot health assessments
Managing Disease Progression
Medication Management
As type 2 diabetes progresses, medication needs often change. Treatment may evolve from oral medications to multiple drug combinations or insulin therapy. Regular medication reviews with healthcare providers ensure optimal treatment effectiveness.
Lifestyle Modifications
Implementing and maintaining healthy lifestyle changes can significantly slow disease progression:
- Following a balanced, diabetes-friendly diet
- Engaging in regular physical activity
- Maintaining a healthy weight
- Managing stress effectively
- Getting adequate sleep
Preventing Complications
Proper management of type 2 diabetes is crucial for preventing serious complications such as:
- Cardiovascular disease
- Kidney damage
- Nerve damage (neuropathy)
- Vision problems
- Foot complications
Frequently Asked Questions
What causes type 2 diabetes to progress over time and how does insulin resistance play a role?
Type 2 diabetes progresses primarily due to increasing insulin resistance and declining pancreatic function. Over time, the body's cells become less responsive to insulin, while the pancreas gradually loses its ability to produce sufficient insulin to maintain normal blood sugar levels.
How can lifestyle changes and medication slow the progression of type 2 diabetes?
Lifestyle modifications like regular exercise, healthy eating, and weight management can help improve insulin sensitivity and reduce the strain on the pancreas. Medications, when taken as prescribed, help control blood sugar levels and protect pancreatic function, thereby slowing disease progression.
What symptoms indicate that type 2 diabetes is worsening or progressing?
Signs of worsening diabetes include increased thirst and urination, persistent fatigue, slower wound healing, frequent infections, blurred vision, and the need for higher medication doses to maintain blood sugar control.
How often should blood sugar levels and treatment plans be monitored and adjusted for type 2 diabetes?
Blood sugar should be monitored daily at home, with A1C tests every 3-6 months. Treatment plans should be reviewed at least quarterly with healthcare providers, with adjustments made based on blood sugar patterns and overall health status.
What complications can develop as type 2 diabetes progresses and blood sugar remains uncontrolled?
Uncontrolled blood sugar can lead to serious complications including heart disease, kidney damage, nerve damage, vision problems, and poor wound healing. Regular monitoring and proper management are essential to prevent these complications.