Prostatitis with swollen lymph nodes represents a significant health concern that requires prompt medical attention. When bacterial prostatitis develops, it can trigger an immune response that affects the lymphatic system, leading to swollen lymph nodes in the groin area. Understanding the connection between these conditions is crucial for proper diagnosis and treatment.
This comprehensive guide explores the relationship between prostatitis and swollen lymph nodes, covering symptoms, diagnosis, causes, and treatment options to help you better understand these interconnected health issues.
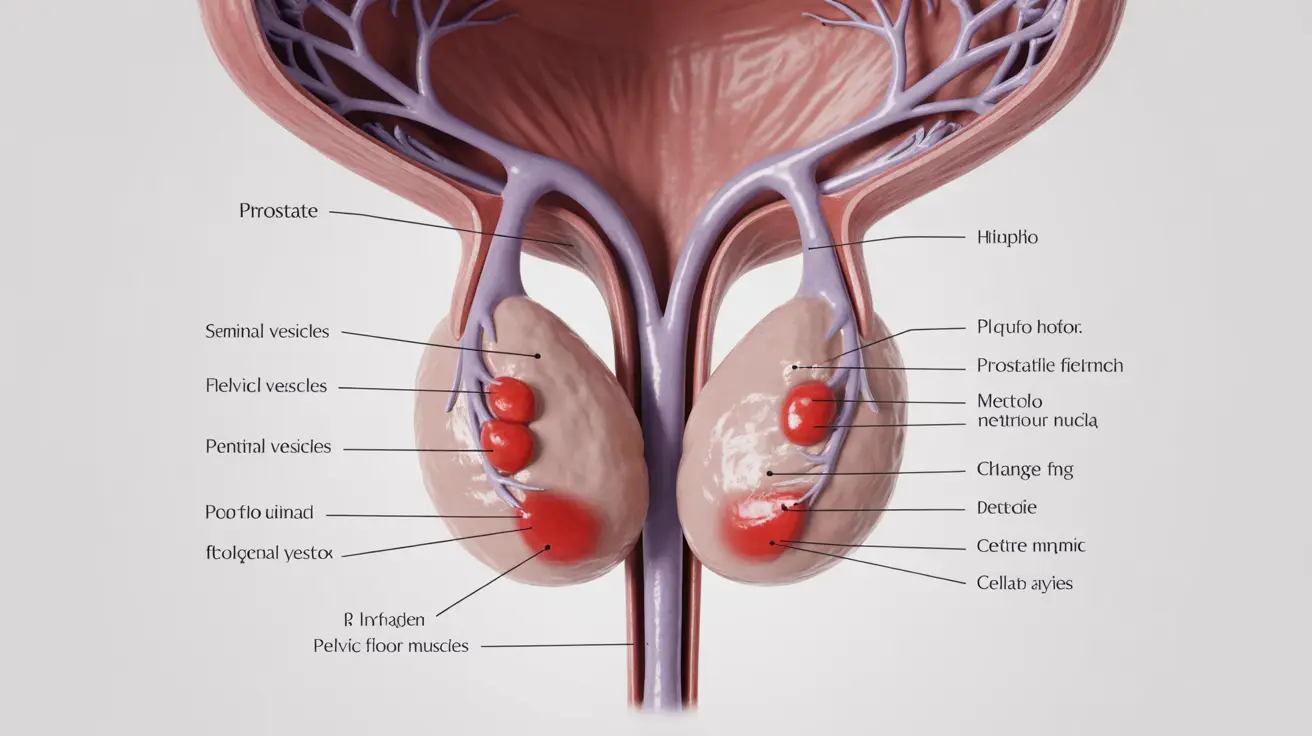
Understanding Prostatitis and Lymph Node Involvement
Acute bacterial prostatitis is a serious infection of the prostate gland that can affect the surrounding lymphatic system. The body's immune response to the infection often results in enlarged lymph nodes, particularly in the groin area, as these nodes work to filter out harmful bacteria and other pathogens.
Key Symptoms and Warning Signs
The combination of prostatitis and swollen lymph nodes typically presents with several distinct symptoms:
- Severe pain in the lower back, pelvic area, or groin
- Difficulty or pain during urination
- Frequent urge to urinate
- Fever and chills
- Noticeable swelling in the groin lymph nodes
- General fatigue and malaise
- Muscle aches and joint pain
Diagnostic Process and Medical Assessment
Healthcare providers use various methods to diagnose prostatitis and evaluate swollen lymph nodes:
- Physical examination of the prostate and lymph nodes
- Urine tests to identify bacterial infections
- Blood tests to check for infection markers
- Digital rectal examination (DRE)
- Imaging studies when necessary
Risk Factors and Causes
Several factors can increase the risk of developing bacterial prostatitis with lymph node involvement:
- Recent urinary tract infections
- Use of urinary catheters
- Previous prostate procedures
- Compromised immune system
- Structural abnormalities in the urinary tract
Treatment Approaches
Treatment typically involves a comprehensive approach targeting both the prostate infection and associated lymph node swelling:
- Antibiotic therapy (usually 2-4 weeks)
- Pain management medications
- Anti-inflammatory drugs
- Rest and increased fluid intake
- Regular monitoring of lymph node status
Prevention Strategies
Taking preventive measures can help reduce the risk of developing prostatitis and associated lymph node complications:
- Maintaining good hygiene
- Staying well-hydrated
- Seeking prompt treatment for urinary tract infections
- Regular health check-ups
- Following prescribed treatment plans completely
Frequently Asked Questions
What are the common symptoms of acute bacterial prostatitis and how are swollen lymph nodes involved?
Common symptoms include severe pelvic pain, fever, difficult urination, and swollen lymph nodes in the groin area. The lymph nodes become enlarged as part of the body's immune response to the infection.
How do doctors diagnose acute bacterial prostatitis and assess swollen lymph nodes in the groin?
Doctors perform physical examinations, including checking lymph node size and tenderness, conduct urine and blood tests, and may use imaging studies to confirm the diagnosis and extent of inflammation.
What causes acute bacterial prostatitis and what risk factors increase the chance of swollen lymph nodes?
Bacterial infections are the primary cause, with risk factors including recent urinary tract infections, catheter use, and compromised immune function. These factors can lead to both prostate infection and lymph node swelling.
What is the recommended treatment for acute bacterial prostatitis with swollen lymph nodes?
Treatment typically includes a course of antibiotics, pain management medications, and anti-inflammatory drugs. The approach addresses both the prostate infection and the associated lymph node swelling.
Can swollen lymph nodes in the groin indicate the severity or spread of prostatitis infection?
Yes, swollen lymph nodes can indicate the severity of the infection and its spread. Their size and tenderness often correlate with the extent of the inflammatory response and may help doctors monitor treatment progress.