Living with ulcerative colitis (UC) presents various challenges, and the development of pseudopolyps is one complication that patients may encounter. These inflammatory growths form in the colon as part of the healing process during periods of inflammation and remission in UC. Understanding what pseudopolyps are, their implications, and how they're managed is crucial for anyone affected by this condition.
While the term "polyp" might sound alarming, pseudopolyps are actually non-cancerous tissue formations that develop as a result of the body's healing response to inflammation. Let's explore everything you need to know about these distinctive features of ulcerative colitis.
What Are Pseudopolyps?
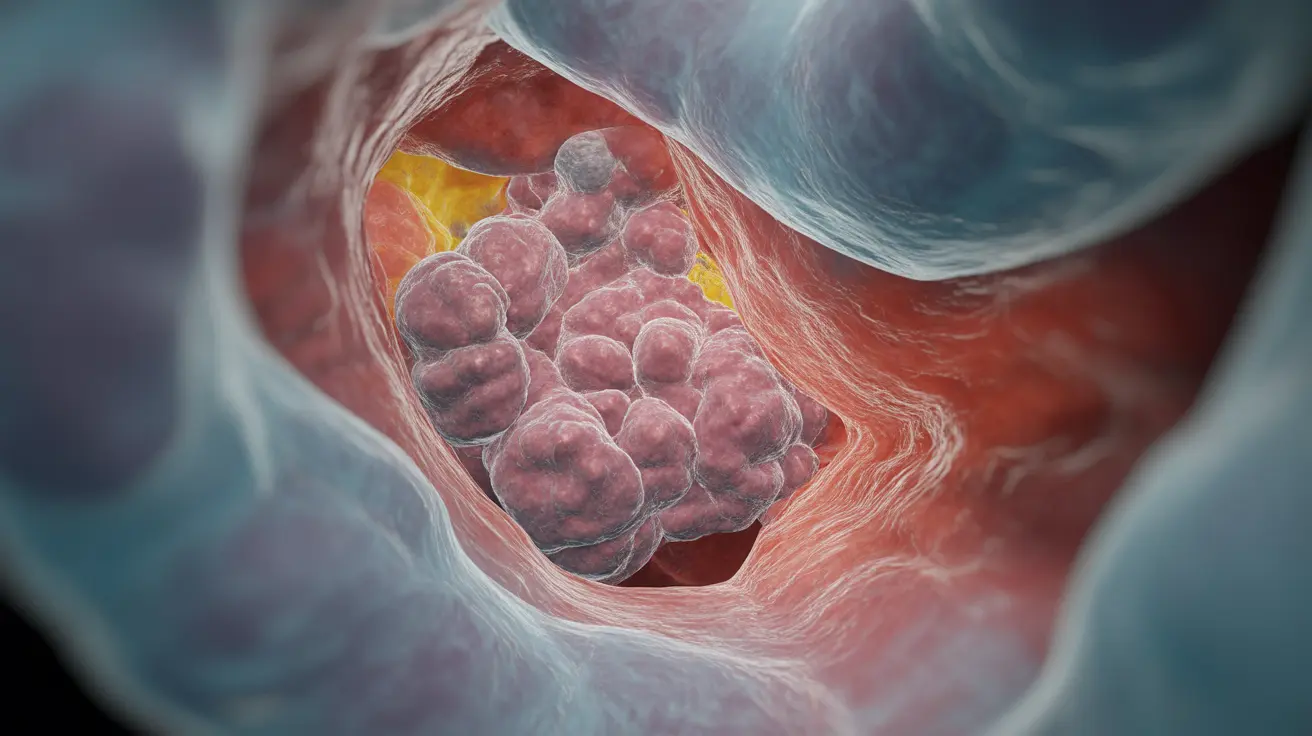
Pseudopolyps are islands of inflamed tissue that remain after surrounding tissue has healed during periods of ulcerative colitis flares. Unlike true polyps, these formations aren't new growth but rather remnants of the inflammatory process. They appear as raised, irregular areas in the colon's lining and can vary in size and number.
These inflammatory markers typically develop in patients who have experienced severe or multiple episodes of inflammation in their colon. They serve as indicators of previous disease activity and can help healthcare providers understand the severity and extent of past inflammation.
Formation and Development
The formation of pseudopolyps occurs through a specific healing pattern in ulcerative colitis. During intense inflammation, some areas of the colon's mucosa become severely damaged while others remain relatively intact. As healing progresses, the preserved areas of tissue can appear as elevated islands surrounded by areas of ulceration, creating these characteristic formations.
Clinical Significance and Monitoring
Healthcare providers pay close attention to pseudopolyps for several reasons. While they themselves are benign, their presence can complicate the monitoring of the colon for more serious developments. Regular surveillance becomes particularly important because pseudopolyps can make it more challenging to detect potentially cancerous growths during colonoscopy.
Diagnosis and Detection
Identifying pseudopolyps typically involves several diagnostic approaches:
- Colonoscopy with high-definition imaging
- Tissue sampling (biopsy) when necessary
- Advanced imaging techniques to distinguish them from other types of growths
- Regular monitoring through follow-up examinations
Management Approaches
The management of pseudopolyps generally focuses on:
- Regular monitoring through scheduled colonoscopies
- Documentation of size, location, and number of pseudopolyps
- Removal when they cause symptoms or interfere with disease monitoring
- Ongoing control of underlying ulcerative colitis
Frequently Asked Questions
What causes pseudopolyps to form in people with ulcerative colitis?
Pseudopolyps form as a result of the healing process following severe inflammation in ulcerative colitis. They represent islands of preserved tissue surrounded by areas that have been damaged and healed, creating raised formations in the colon's lining.
What symptoms can pseudopolyps cause, and when do they become a problem?
Most pseudopolyps don't cause symptoms on their own. However, they can become problematic if they're large or numerous enough to cause obstruction, bleeding, or interfere with proper disease monitoring. They may also make it more difficult to detect other concerning changes in the colon.
How are pseudopolyps diagnosed and distinguished from cancerous polyps?
Diagnosis typically involves colonoscopy with high-definition imaging. Healthcare providers can usually distinguish pseudopolyps from cancerous growths based on their characteristic appearance, but biopsies may be necessary in some cases. Their scattered, irregular pattern and relationship to areas of previous inflammation help identify them as pseudopolyps.
Do pseudopolyps increase the risk of colon cancer in ulcerative colitis patients?
Pseudopolyps themselves don't directly increase cancer risk. However, their presence often indicates a history of severe inflammation, which is associated with an increased risk of colorectal cancer. They can also make cancer surveillance more challenging by obscuring other growths.
What treatment options are available if pseudopolyps lead to complications?
When pseudopolyps cause complications or significantly interfere with disease monitoring, they may need to be removed through endoscopic procedures. The primary focus remains on controlling the underlying ulcerative colitis through appropriate medical management to prevent new pseudopolyp formation.