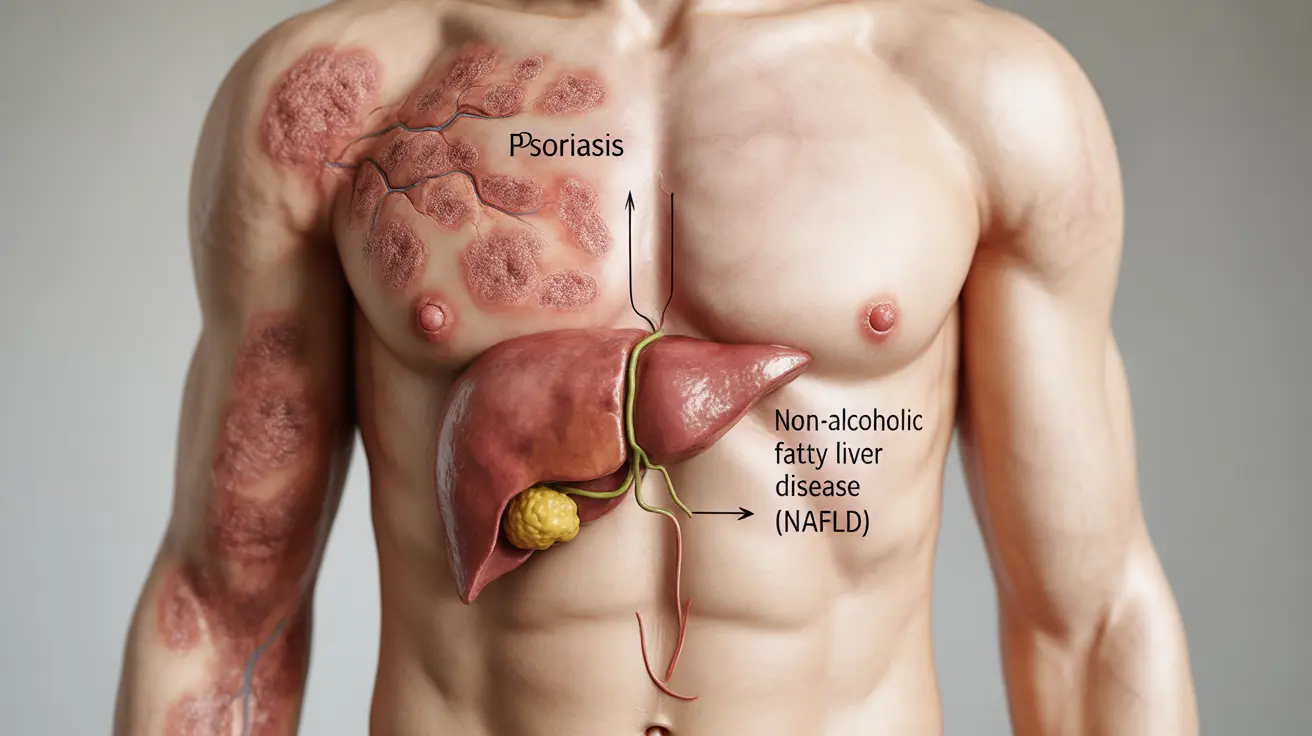
The relationship between psoriasis and liver disease represents an important yet often overlooked connection in medical science. As researchers continue to uncover links between these conditions, understanding their interaction becomes crucial for both patients and healthcare providers.
Recent studies have shown that individuals with psoriasis may face an increased risk of developing various liver conditions, particularly non-alcoholic fatty liver disease (NAFLD). This guide explores the complex relationship between these conditions and provides essential information for managing both effectively.
The Connection Between Psoriasis and Liver Disease
Psoriasis and liver disease share several common inflammatory pathways. The chronic inflammation associated with psoriasis can affect multiple organ systems, including the liver. This systemic inflammation may contribute to the development or progression of liver conditions.
Research indicates that people with psoriasis have a higher prevalence of non-alcoholic fatty liver disease compared to the general population. This connection appears to be influenced by shared risk factors and inflammatory processes.
Common Types of Liver Disease in Psoriasis Patients
Non-Alcoholic Fatty Liver Disease (NAFLD)
NAFLD is particularly common among psoriasis patients, characterized by excessive fat accumulation in the liver. This condition can be influenced by factors such as obesity, metabolic syndrome, and chronic inflammation.
Drug-Induced Liver Injury
Some psoriasis treatments, particularly certain systemic medications, can affect liver function. Understanding these risks is crucial for proper disease management and monitoring.
Recognizing Liver Disease Symptoms
Early detection of liver problems is essential for psoriasis patients. Key symptoms to watch for include:
- Fatigue and weakness
- Jaundice (yellowing of skin or eyes)
- Abdominal pain or swelling
- Dark urine
- Unexplained weight loss
- Nausea or vomiting
Treatment Considerations and Medication Safety
Managing psoriasis while protecting liver health requires careful consideration of treatment options. Healthcare providers must balance the effectiveness of psoriasis treatments with potential liver risks.
Monitoring Liver Function
Regular liver function testing is essential for patients on systemic psoriasis medications. The frequency of monitoring depends on the specific medication and individual risk factors.
Lifestyle Modifications for Better Management
Adopting healthy lifestyle choices can help manage both conditions effectively:
- Maintaining a healthy weight
- Following a balanced, anti-inflammatory diet
- Limiting alcohol consumption
- Regular exercise
- Stress management
- Adequate sleep
Frequently Asked Questions
What is the connection between psoriasis and liver disease, especially fatty liver disease?
Psoriasis and liver disease share inflammatory pathways, with psoriasis patients showing a higher risk of developing non-alcoholic fatty liver disease. The connection is primarily due to shared inflammatory mechanisms and metabolic factors.
How do psoriasis medications like methotrexate affect the risk of liver damage?
Some psoriasis medications, particularly methotrexate, can potentially cause liver damage. This risk requires regular monitoring of liver function and may influence treatment choices based on individual patient factors.
What are the symptoms of liver disease in people who have psoriasis?
Common symptoms include fatigue, jaundice, abdominal pain, dark urine, and unexplained weight changes. These symptoms may develop gradually and require prompt medical attention when noticed.
How can lifestyle changes help reduce liver disease risk in patients with psoriasis?
Maintaining a healthy weight, following an anti-inflammatory diet, limiting alcohol, exercising regularly, and managing stress can help reduce liver disease risk in psoriasis patients.
What liver function monitoring is recommended for psoriasis patients on systemic treatments?
Regular liver function tests are typically required, with frequency varying based on the medication type and individual risk factors. Initial baseline testing and ongoing monitoring are standard practices for patients on systemic treatments.