Psoriatic arthritis is a complex autoimmune condition that affects millions of people worldwide, causing joint pain, stiffness, and inflammation alongside skin symptoms. Unlike some other forms of arthritis, diagnosing psoriatic arthritis can be challenging because there's no single definitive test that confirms the condition. Understanding what blood tests are involved in the diagnostic process can help you better prepare for your medical appointments and know what to expect.
While blood tests play an important supporting role in diagnosing psoriatic arthritis, they're typically used in combination with physical examinations, medical history, and imaging studies to paint a complete picture of your condition. Let's explore how these diagnostic tools work together to help healthcare providers identify and treat this inflammatory arthritis condition.
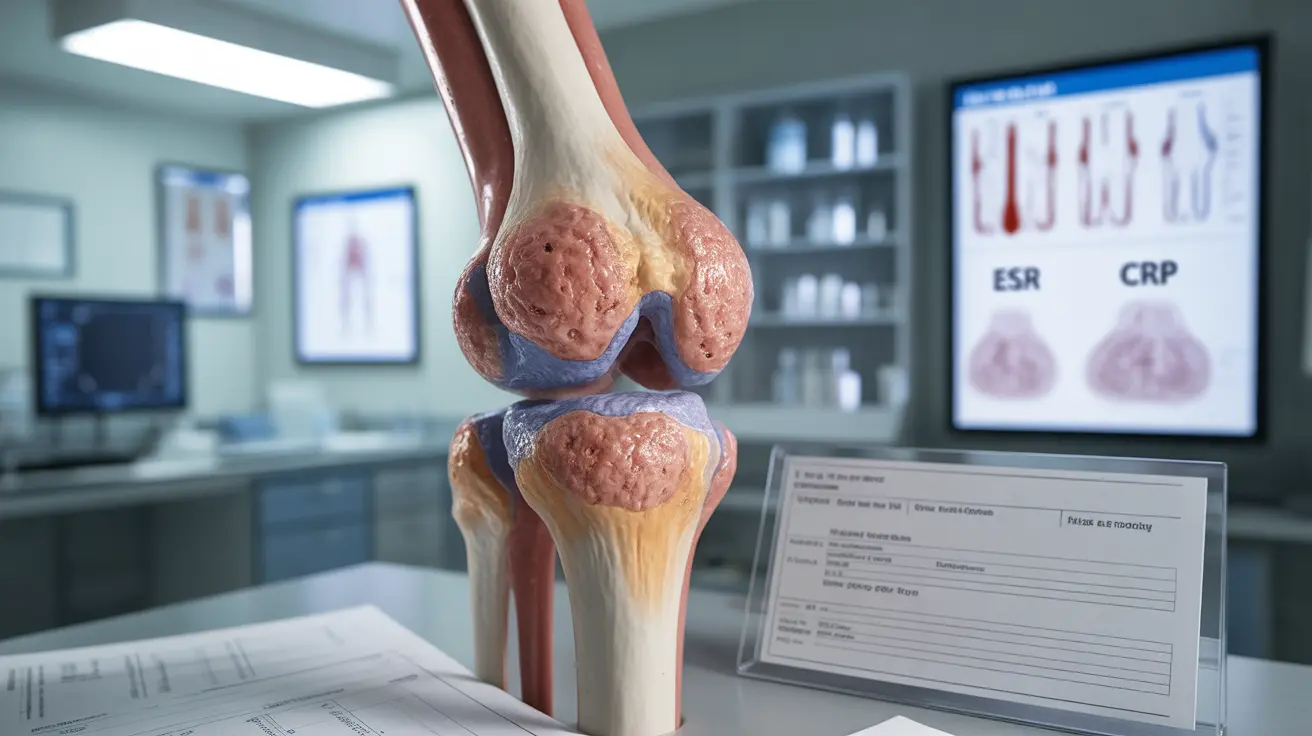
Understanding Blood Tests in Psoriatic Arthritis Diagnosis
When doctors suspect psoriatic arthritis, they typically order several blood tests to rule out other conditions and look for signs of inflammation. These tests don't directly confirm psoriatic arthritis, but they provide valuable information that helps healthcare providers make an accurate diagnosis.
The most commonly ordered blood tests include inflammatory markers like erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which can indicate the presence of systemic inflammation in your body. Elevated levels of these markers suggest that your immune system is actively fighting something, which is consistent with autoimmune conditions like psoriatic arthritis.
Complete blood count (CBC) tests are also routinely performed to check for anemia or other blood-related abnormalities that sometimes accompany chronic inflammatory conditions. Additionally, doctors may test your liver and kidney function, especially if they're considering certain medications for treatment.
The Role of Rheumatoid Factor Testing
One of the most significant aspects of psoriatic arthritis blood testing involves checking for rheumatoid factor (RF), an antibody that's commonly found in people with rheumatoid arthritis. Interestingly, most people with psoriatic arthritis test negative for rheumatoid factor, which actually helps doctors distinguish between these two similar conditions.
A negative rheumatoid factor test, combined with the presence of psoriasis and joint symptoms, strongly suggests psoriatic arthritis rather than rheumatoid arthritis. This distinction is crucial because the two conditions require different treatment approaches and have different long-term outlooks.
Healthcare providers may also test for anti-cyclic citrullinated peptide (anti-CCP) antibodies, which are another marker typically associated with rheumatoid arthritis. Like rheumatoid factor, anti-CCP antibodies are usually absent in people with psoriatic arthritis.
Genetic Testing and HLA-B27
Some doctors may order genetic testing to look for the HLA-B27 gene, which is found in about 20% of people with psoriatic arthritis, particularly those who develop spinal involvement. While having this gene doesn't mean you'll definitely develop the condition, its presence can support a diagnosis when combined with other clinical findings.
It's important to understand that genetic testing is not routinely necessary for diagnosing psoriatic arthritis, and many people with the condition don't carry the HLA-B27 gene. Your doctor will determine whether this test is appropriate based on your specific symptoms and family history.
Recognizing Symptoms Beyond Joint Pain
While blood tests provide valuable diagnostic information, recognizing the full spectrum of psoriatic arthritis symptoms is equally important. Beyond the characteristic joint pain and stiffness, many people experience skin symptoms including red, scaly patches typical of psoriasis. These skin changes may appear before, during, or after joint symptoms develop.
Nail changes are another common sign of psoriatic arthritis that many people overlook. These can include pitting (small dents), ridging, thickening, or separation of the nail from the nail bed. Eye inflammation, called uveitis, can also occur and requires prompt medical attention to prevent complications.
Fatigue is a frequently reported symptom that can significantly impact daily life. This overwhelming tiredness goes beyond normal fatigue and often doesn't improve with rest. Some people also experience enthesitis, which is inflammation where tendons and ligaments attach to bones, commonly affecting the heels and bottoms of feet.
The Diagnostic Process
Diagnosing psoriatic arthritis requires a comprehensive approach that goes far beyond blood tests alone. Your healthcare provider will conduct a thorough physical examination, looking for swollen joints, skin changes, and nail abnormalities. They'll also review your personal and family medical history, paying particular attention to any history of psoriasis or other autoimmune conditions.
Imaging studies, such as X-rays, ultrasounds, or MRI scans, help doctors visualize joint damage and inflammation that may not be apparent during a physical exam. These tests can reveal characteristic changes in the joints and spine that support a psoriatic arthritis diagnosis.
The combination of clinical symptoms, physical examination findings, blood test results, and imaging studies helps doctors make an accurate diagnosis. This comprehensive approach is necessary because psoriatic arthritis can mimic other conditions and varies significantly from person to person.
Frequently Asked Questions
What blood tests are used to diagnose psoriatic arthritis?
Common blood tests for psoriatic arthritis include inflammatory markers like ESR and CRP, complete blood count (CBC), rheumatoid factor, anti-CCP antibodies, and sometimes HLA-B27 genetic testing. These tests help rule out other conditions and detect inflammation but don't definitively diagnose psoriatic arthritis on their own.
Can a blood test alone confirm psoriatic arthritis?
No, there is no single blood test that can definitively confirm psoriatic arthritis. Diagnosis requires a combination of blood tests, physical examination, medical history, and often imaging studies. Blood tests primarily help exclude other conditions and detect inflammation rather than providing a definitive diagnosis.
What does a negative rheumatoid factor mean for psoriatic arthritis?
A negative rheumatoid factor test actually supports a psoriatic arthritis diagnosis, as most people with this condition test negative for RF. This helps doctors distinguish psoriatic arthritis from rheumatoid arthritis, where RF is typically positive. The absence of rheumatoid factor is considered a characteristic feature of psoriatic arthritis.
How do doctors differentiate psoriatic arthritis from rheumatoid arthritis with blood tests?
Doctors look for negative rheumatoid factor and anti-CCP antibodies in psoriatic arthritis, whereas these markers are usually positive in rheumatoid arthritis. Additionally, inflammatory markers may show different patterns, and genetic testing for HLA-B27 may be positive in some psoriatic arthritis cases but not in rheumatoid arthritis.
What are the most common symptoms and signs of psoriatic arthritis besides joint pain?
Common symptoms include skin psoriasis with red, scaly patches; nail changes like pitting or thickening; fatigue; eye inflammation (uveitis); enthesitis (inflammation where tendons attach to bones); and morning stiffness. Some people also experience lower back pain and stiffness, particularly if the spine is involved.