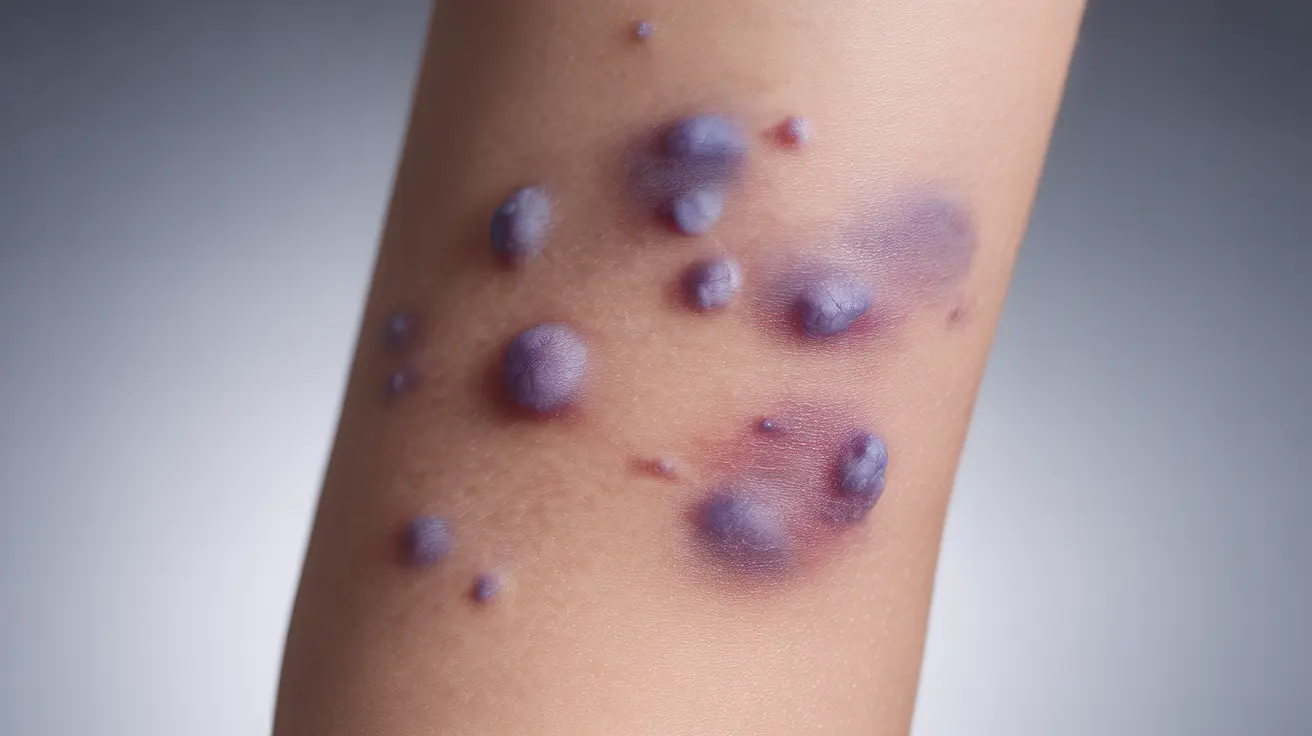
Purpura, a distinctive skin manifestation characterized by purple spots or patches, plays a crucial role in identifying and understanding Thrombotic Thrombocytopenic Purpura (TTP). This rare but serious blood disorder affects the body's blood clotting system and requires immediate medical attention. Understanding how purpura develops and its significance in TTP can help both patients and healthcare providers identify and manage this condition effectively.
The Connection Between Purpura and TTP
In TTP, purpura develops due to a complex chain of events within the blood vessels. When blood platelets form abnormal clots throughout the body, it leads to a significant decrease in platelet count. This reduction in platelets, known as thrombocytopenia, results in the characteristic purpura – visible as purple bruising or spots on the skin.
Understanding the Mechanism of Purpura Formation
The development of purpura in TTP occurs when small blood vessels become damaged, allowing blood to leak into surrounding tissues. This process happens because of two main factors:
- Widespread formation of microscopic blood clots
- Severe reduction in platelet count
- Damage to small blood vessels
Recognizing TTP Symptoms Beyond Purpura
While purpura is a hallmark sign of TTP, the condition presents with several other important symptoms that patients and healthcare providers should monitor:
Physical Symptoms
- Purple bruising or spots (purpura)
- Unexplained bruising
- Petechiae (tiny red or purple spots)
- Paleness or jaundice
- Fatigue and weakness
Neurological Symptoms
- Confusion or disorientation
- Headaches
- Speech changes
- Seizures
Diagnostic Approach for TTP
When purpura is present, healthcare providers will initiate a comprehensive diagnostic process to confirm TTP:
- Complete blood count (CBC)
- Blood smear examination
- ADAMTS13 activity testing
- Kidney and liver function tests
Treatment Options and Management
The presence of purpura often signals the need for immediate treatment of TTP. Current treatment approaches include:
Primary Treatments
- Plasma exchange (plasmapheresis)
- Rituximab therapy
- Corticosteroids
- Blood transfusions when necessary
Supportive Care
- Regular monitoring of platelet counts
- Management of complications
- Prevention of bleeding
Monitoring and Prevention of Recurrence
After initial treatment, ongoing monitoring is essential to prevent and detect potential relapses. This includes regular blood tests and awareness of early warning signs, particularly the reappearance of purpura.
Frequently Asked Questions
- What causes purpura in thrombotic thrombocytopenic purpura (TTP) and how is it related to low platelet counts?
Purpura in TTP occurs when abnormally low platelet counts (thrombocytopenia) result from widespread clotting in small blood vessels. The lack of available platelets leads to easy bruising and bleeding under the skin, creating the characteristic purple spots or patches known as purpura.
- What are the common symptoms and signs of TTP that include purpura or bleeding under the skin?
Common signs include purple bruising (purpura), tiny red or purple spots (petechiae), unexplained bruising, pale skin, fatigue, and possible neurological symptoms such as confusion or headaches.
- How is thrombotic thrombocytopenic purpura diagnosed, especially when purpura is present?
Diagnosis involves a combination of clinical observation of purpura and other symptoms, blood tests including complete blood count, ADAMTS13 activity testing, and examination of blood smears to evaluate platelet levels and detect abnormal blood cell patterns.
- What treatments are available to manage TTP and reduce symptoms like purpura?
Primary treatments include plasma exchange (plasmapheresis), rituximab therapy, corticosteroids, and blood transfusions when necessary. Treatment aims to restore normal platelet levels and resolve symptoms including purpura.
- Can purpura from TTP come back after treatment, and what should patients watch for to detect relapses?
Yes, purpura can recur if TTP relapses. Patients should monitor for the reappearance of purple spots or bruising, unusual bleeding, fatigue, and neurological symptoms. Regular medical follow-up and blood tests help detect early signs of recurrence.