Pyloroplasty surgery is a specialized surgical procedure that modifies the pylorus, a muscular valve between the stomach and small intestine. This important operation helps patients who experience difficulties with stomach emptying by widening the pyloric channel, allowing food to pass more easily from the stomach into the small intestine.
For individuals suffering from conditions like gastroparesis or pyloric stenosis, this procedure can be life-changing, offering relief from chronic symptoms and improving overall quality of life. Understanding what the surgery entails, its benefits, and recovery process is crucial for patients considering this treatment option.
What Is Pyloroplasty and How Does It Work?
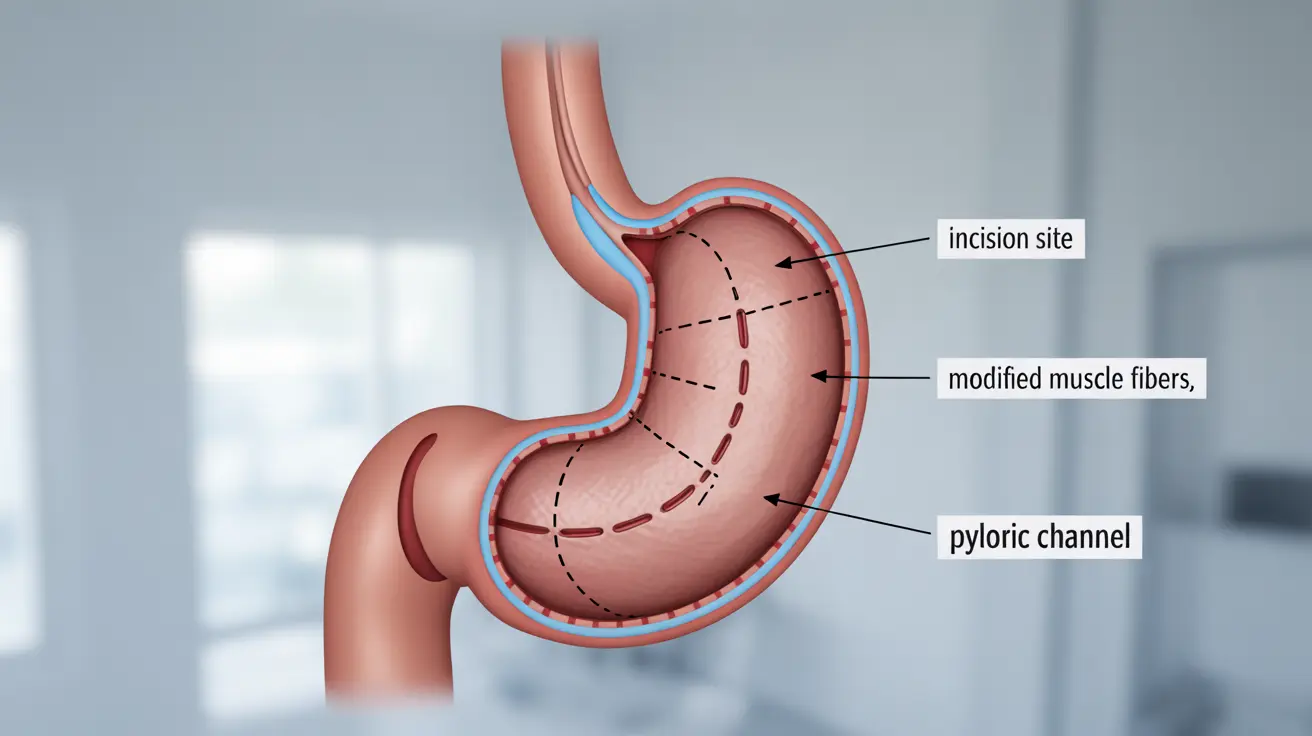
Pyloroplasty involves surgically altering the pylorus to create a wider opening between the stomach and small intestine. The procedure works by making an incision in the pyloric muscle and reconstructing it in a way that prevents it from becoming too narrow or tight, ensuring proper stomach emptying.
The surgery addresses various conditions that affect gastric emptying, particularly those where the pyloric sphincter doesn't function correctly or has become too narrow to allow normal passage of food.
Conditions Treated with Pyloroplasty
Several medical conditions may necessitate pyloroplasty surgery:
- Gastroparesis (delayed stomach emptying)
- Pyloric stenosis
- Peptic ulcer disease complications
- Gastric outlet obstruction
Surgical Techniques and Approaches
Laparoscopic Pyloroplasty
Modern surgical techniques often utilize laparoscopic approaches, which involve making several small incisions in the abdomen. Through these openings, surgeons insert specialized instruments and a camera to perform the procedure. This minimally invasive approach typically results in:
- Shorter hospital stays
- Reduced post-operative pain
- Faster recovery time
- Smaller scars
Open Pyloroplasty
In some cases, traditional open surgery may be necessary. This approach involves making a larger incision in the abdomen to access the pylorus directly. While this method may require longer recovery time, it can be the better option for certain patients, particularly those with complex medical histories or anatomical considerations.
Preparing for Surgery
Before undergoing pyloroplasty, patients typically need to:
- Complete comprehensive medical evaluations
- Undergo specific diagnostic tests
- Follow fasting guidelines
- Adjust or temporarily stop certain medications
- Arrange for post-operative care and support
Recovery and Post-Operative Care
Recovery from pyloroplasty requires careful attention to post-operative instructions. Patients typically progress through several stages:
- Initial recovery in the hospital (2-4 days)
- Gradual return to normal activities
- Dietary modifications and restrictions
- Regular follow-up appointments
- Monitoring for potential complications
Frequently Asked Questions
What is pyloroplasty surgery and why is it performed?
Pyloroplasty surgery is a procedure that widens the opening between the stomach and small intestine by modifying the pyloric sphincter. It's performed to treat conditions that prevent proper stomach emptying, such as gastroparesis or pyloric stenosis, helping patients who experience chronic nausea, vomiting, and difficulty eating.
How is pyloroplasty surgery done and what are the differences between open and laparoscopic techniques?
Pyloroplasty can be performed either through traditional open surgery or laparoscopically. Laparoscopic surgery uses small incisions and specialized instruments, offering faster recovery and less scarring. Open surgery requires a larger incision but may be necessary for complex cases or when better visualization is needed.
What conditions can be treated with pyloroplasty surgery?
Pyloroplasty treats several conditions including gastroparesis, pyloric stenosis, complications from peptic ulcer disease, and gastric outlet obstruction. These conditions all involve problems with food passing from the stomach to the small intestine.
What are the common risks and possible complications after pyloroplasty surgery?
Common risks include infection, bleeding, delayed healing, temporary digestive issues, and reaction to anesthesia. Less common complications might include leakage at the surgical site, bowel obstruction, or dumping syndrome. However, serious complications are relatively rare when the procedure is performed by experienced surgeons.
How long does recovery take after pyloroplasty and what should I expect during the healing process?
Recovery typically takes 4-6 weeks for full healing. Initially, patients stay in the hospital for 2-4 days, followed by a graduated diet progression from liquids to solid foods. Most patients can return to normal activities within 2-3 weeks, though heavy lifting and strenuous exercise should be avoided for 4-6 weeks.