The connection between COVID-19 and reactive arthritis has emerged as an important area of study as medical professionals continue to understand the various post-viral complications of SARS-CoV-2 infection. Reactive arthritis is an inflammatory condition that can develop following certain infections, including COVID-19, affecting joints and causing significant discomfort.
This comprehensive guide explores the relationship between COVID-19 and reactive arthritis, including symptoms, diagnosis, treatment options, and potential long-term implications for patients.
Symptoms and Timeline of Post-COVID Reactive Arthritis
Reactive arthritis following COVID-19 typically develops within several days to a few weeks after the initial infection. The condition presents with several characteristic symptoms:
- Joint pain and swelling, particularly in larger joints
- Morning stiffness lasting more than 30 minutes
- Lower back pain
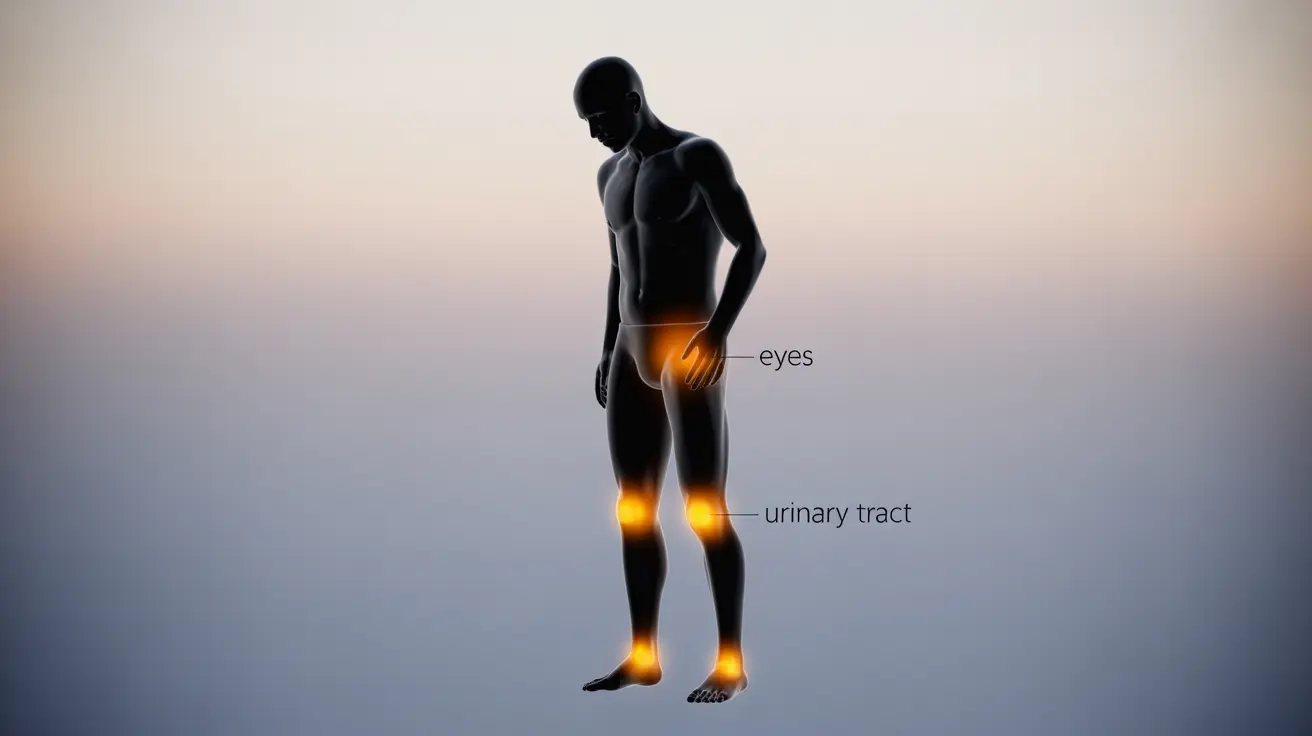
- Inflammation in the knees, ankles, or feet
- Potential involvement of eyes and urinary tract
Unlike typical COVID-19 symptoms, reactive arthritis manifestations are specifically related to joint inflammation and can persist for weeks or months after the viral infection has resolved.
Diagnostic Process and Clinical Evaluation
Diagnosing reactive arthritis after COVID-19 requires careful clinical evaluation and various diagnostic tools:
- Physical examination of affected joints
- Blood tests for inflammatory markers
- Imaging studies (X-rays, MRI)
- Testing for COVID-19 antibodies
- Synovial fluid analysis when necessary
Healthcare providers must differentiate reactive arthritis from other post-COVID complications and similar rheumatic conditions to ensure appropriate treatment.
Treatment Approaches and Management Strategies
The treatment of COVID-related reactive arthritis typically involves a multi-faceted approach:
Medication Options
- Nonsteroidal anti-inflammatory drugs (NSAIDs)
- Corticosteroid injections for severe cases
- Disease-modifying antirheumatic drugs (DMARDs) when necessary
Physical Therapy and Self-Care
Physical therapy plays a crucial role in managing symptoms and maintaining joint function. Self-care measures may include:
- Regular gentle exercise
- Hot and cold therapy
- Range-of-motion exercises
- Adequate rest during flare-ups
Long-Term Outlook and Prognosis
The long-term impact of COVID-induced reactive arthritis varies among individuals. While many patients experience improvement within 3-12 months, some may develop chronic symptoms requiring ongoing management. Regular monitoring and adjusting treatment plans as needed are essential for optimal outcomes.
Genetic Factors and Risk Assessment
The role of genetic factors, particularly the HLA-B27 gene, in post-COVID reactive arthritis is still being studied. While this gene is associated with various forms of inflammatory arthritis, its specific influence on COVID-related cases requires further research.
Frequently Asked Questions
What are the typical symptoms and onset time of reactive arthritis after a COVID-19 infection?
Reactive arthritis typically develops within 1-4 weeks after COVID-19 infection. Common symptoms include joint pain and swelling, particularly in larger joints, morning stiffness, and potential inflammation in eyes or urinary tract.
How is reactive arthritis caused by COVID-19 diagnosed and differentiated from other joint conditions?
Diagnosis involves physical examination, blood tests for inflammatory markers, imaging studies, and careful consideration of the patient's COVID-19 history. Doctors must rule out other rheumatic conditions through differential diagnosis.
What treatments are effective for managing reactive arthritis following COVID-19 infection?
Effective treatments include NSAIDs, corticosteroid injections for severe cases, physical therapy, and in some cases, DMARDs. Treatment plans are typically individualized based on symptom severity and patient response.
Can reactive arthritis triggered by COVID-19 cause long-term joint problems or disability?
While most cases resolve within 3-12 months, some patients may experience longer-term joint issues. Regular monitoring and appropriate treatment can help prevent or minimize long-term complications.
Is having the HLA-B27 gene a risk factor for developing reactive arthritis after COVID-19?
While HLA-B27 is associated with various forms of inflammatory arthritis, its specific role in COVID-related reactive arthritis is still being researched. Having the gene may influence susceptibility, but more studies are needed for definitive conclusions.