Real milk ducts play a vital role in breast anatomy and function, particularly during pregnancy and lactation. These intricate networks of tubes are essential components of the mammary system, responsible for carrying milk from the milk-producing glands to the nipple during breastfeeding. Understanding how these ducts work and recognizing potential issues can help nursing mothers and those concerned about breast health.
Anatomy and Structure of Milk Ducts
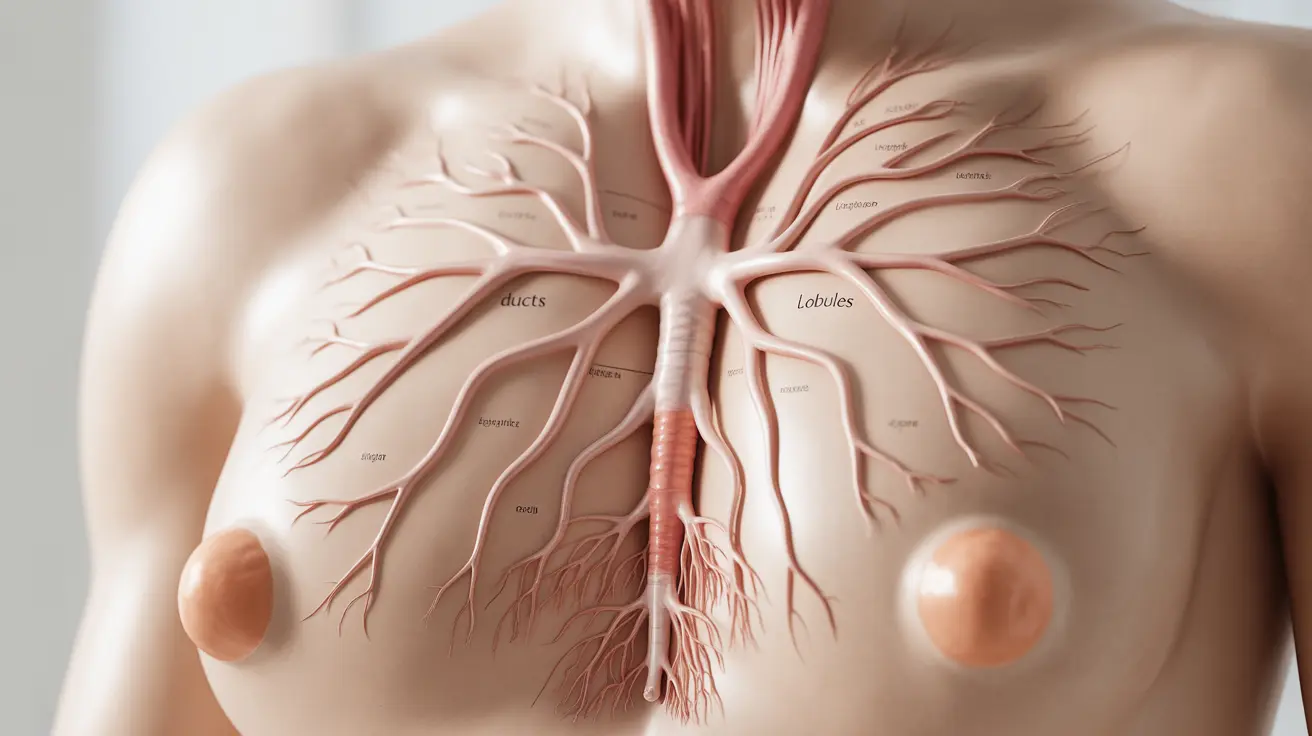
The breast contains a complex system of milk ducts arranged in a tree-like pattern. These ducts begin at the milk-producing lobules and gradually merge into larger ducts, ultimately connecting to the nipple through 15-20 main ducts. The entire network is supported by surrounding breast tissue and responds to hormonal changes throughout a woman's life.
Normal Function and Development
During puberty, milk ducts undergo their initial development under the influence of hormones like estrogen. However, they remain relatively dormant until pregnancy, when they begin preparing for their primary function of milk production and transport.
Hormonal Influence on Milk Ducts
Several hormones affect milk duct development and function:
- Estrogen promotes duct growth and branching
- Progesterone stimulates lobule development
- Prolactin triggers milk production
- Oxytocin causes milk ejection during breastfeeding
Changes During Pregnancy and Lactation
During pregnancy, milk ducts undergo significant changes to prepare for breastfeeding. They increase in size and number, creating an expanded network capable of handling milk production. The tissue becomes more specialized, with cells specifically designed for milk synthesis and transport.
Postpartum Changes
After childbirth, the milk ducts become fully functional, actively transporting milk from the lobules to the nipple. This system responds to the baby's feeding demands, adjusting milk production and flow accordingly.
Common Milk Duct Issues
Several conditions can affect milk ducts:
- Blocked ducts: Often caused by incomplete milk drainage
- Mastitis: Inflammation or infection of the breast tissue
- Galactoceles: Milk-filled cysts
- Ductal ectasia: Widening and hardening of ducts
Prevention and Treatment
Regular breast emptying during feeding, proper positioning while nursing, and maintaining good breast health can help prevent many common duct-related problems. Early intervention for any issues is crucial to maintain successful breastfeeding.
Ductal Carcinoma and Breast Cancer
Ductal carcinoma is a type of breast cancer that begins in the milk ducts. It can be either non-invasive (DCIS) or invasive (IDC), with different treatment approaches required for each type. Regular screening and early detection are essential for successful treatment outcomes.
Frequently Asked Questions
What are the main functions of real milk ducts in the breast? Real milk ducts serve as transport channels for breast milk, carrying it from the milk-producing lobules to the nipple. They also help regulate milk production and release through hormonal signaling.
How do milk ducts change during pregnancy and breastfeeding? During pregnancy, milk ducts multiply and expand in preparation for lactation. They become more complex and specialized, developing cells specifically designed for milk production and transport.
What causes blockages or infections in the milk ducts? Blockages can occur from incomplete milk drainage, pressure on the breasts, or inflammatory conditions. Poor drainage can lead to bacterial growth and infection, resulting in conditions like mastitis.
How is ductal carcinoma different from other types of breast cancer? Ductal carcinoma specifically originates in the milk ducts, while other types may begin in different breast tissues. It can be non-invasive (contained within the ducts) or invasive (spreading beyond the ducts).
Can milk ducts continue to produce milk if breastfeeding stops and then resumes? Yes, milk ducts can often resume milk production even after a break in breastfeeding, though the amount may vary. This process, called relactation, depends on various factors including the length of the break and hormonal stimulation.