Scar tissue pain can significantly impact daily life, affecting mobility and comfort long after an injury or surgery has healed. This common but often misunderstood condition requires proper attention and management to prevent chronic discomfort and maintain quality of life. Understanding the causes, symptoms, and treatment options is crucial for anyone dealing with painful scar tissue.
Whether you're recovering from surgery, dealing with an old injury, or experiencing unexpected pain in a healed scar, this guide will help you understand why scar tissue can become painful and what you can do about it.
Understanding Scar Tissue Formation and Pain
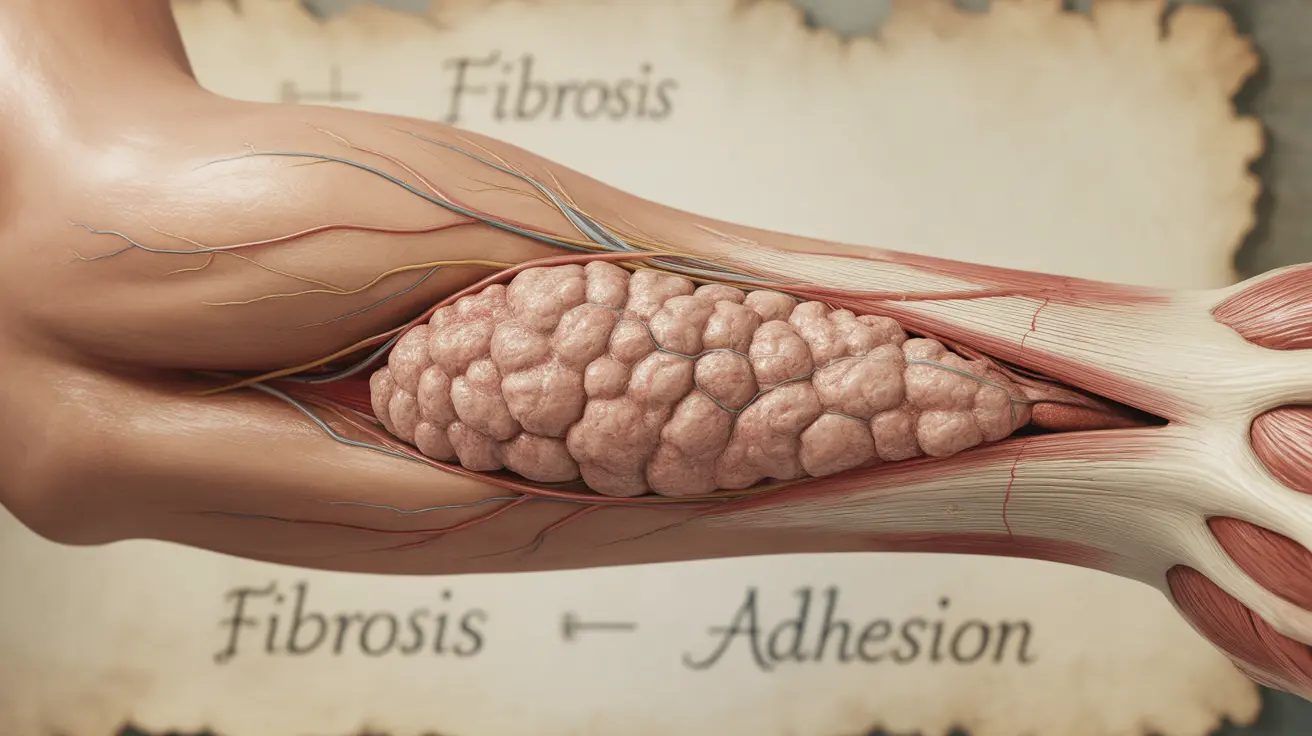
Scar tissue forms as part of the body's natural healing process after injury, surgery, or inflammation. Unlike normal tissue, scar tissue has a different cellular structure and less flexibility, which can lead to various complications and discomfort.
When scar tissue develops, it can adhere to surrounding tissues, muscles, or organs, creating tension and restricted movement. This adhesion often results in pain, particularly during movement or when pressure is applied to the area.
Common Causes of Scar Tissue Pain
Several factors can contribute to pain in scar tissue:
- Adhesions to surrounding tissues
- Nerve entrapment within the scar
- Excessive scar tissue formation
- Poor wound healing
- Infection during the healing process
- Physical strain or overuse of the affected area
Treatment Options for Scar Tissue Pain
Conservative Management Approaches
Many people find relief through non-invasive treatment methods:
- Gentle massage therapy
- Compression garments
- Silicone sheets or gels
- Heat and cold therapy
- Stretching exercises
- Over-the-counter pain medications
Professional Medical Interventions
When conservative treatments aren't sufficient, medical professionals may recommend:
- Physical therapy
- Ultrasound therapy
- Steroid injections
- Scar revision surgery
- Laser therapy
- Medical adhesion release
Prevention and Long-term Management
Taking proper care of wounds and surgical sites from the beginning can help minimize scar tissue problems:
- Following post-operative care instructions carefully
- Keeping the wound clean and properly dressed
- Avoiding excessive movement during initial healing
- Using sun protection on healing scars
- Maintaining proper nutrition for optimal healing
- Starting gentle movement as advised by healthcare providers
Frequently Asked Questions
What are the typical symptoms that indicate scar tissue pain after surgery or injury?
Scar tissue pain typically manifests as tenderness, burning sensations, shooting pains, or a feeling of tightness around the scar. You may also experience reduced range of motion, stiffness, and increased sensitivity to touch or pressure in the affected area.
How can at-home treatments like massage and compression help relieve scar tissue pain?
Massage helps break down adhesions and improve circulation to the scar tissue, while compression can help prevent excessive scar formation and reduce swelling. These techniques, when performed correctly and consistently, can help soften scar tissue and improve flexibility.
What medical procedures are available to reduce pain and improve mobility caused by scar tissue?
Medical procedures include minimally invasive techniques like steroid injections and laser therapy, as well as more extensive treatments such as scar revision surgery. These procedures aim to break down excessive scar tissue and release adhesions that cause pain and restricted movement.
Why does scar tissue sometimes cause pain or stiffness months or years after the initial wound has healed?
Long-term pain can occur due to continued adhesion formation, nerve entrapment within the scar tissue, or changes in tissue mobility over time. Environmental factors, physical activity, and natural aging can also affect how scar tissue responds and potentially cause delayed onset of pain.
How does physical therapy help in managing chronic pain and limited movement due to scar tissue?
Physical therapy employs specialized techniques like manual therapy, targeted exercises, and stretching to improve tissue mobility and reduce pain. Therapists can also teach self-management strategies and provide guidance on appropriate activity modification to prevent further complications.