Back pain affects millions of Americans, with two of the most common culprits being sciatica and arthritis. While both conditions can cause significant discomfort and impact daily activities, they originate from different sources and require distinct treatment approaches. Understanding the relationship between these conditions is crucial for proper diagnosis and effective management.
Many people experience confusion when trying to differentiate between sciatica and arthritis pain, especially when both conditions affect the lower back and spine. The complexity increases when arthritis in the spine contributes to sciatic nerve compression, creating a challenging diagnostic puzzle that requires professional medical evaluation.
What Is Sciatica?
Sciatica refers to pain that radiates along the path of the sciatic nerve, which runs from the lower back through the hips and buttocks and down each leg. This condition typically affects only one side of the body and occurs when the sciatic nerve becomes compressed or irritated.
The sciatic nerve is the longest and widest nerve in the human body, making it particularly susceptible to compression from various spinal conditions. When pressure is applied to this nerve, it can cause sharp, shooting pain, numbness, tingling, or weakness that travels from the lower back down to the foot.
Common causes of sciatica include herniated discs, spinal stenosis, bone spurs, and muscle inflammation. The pain pattern is distinctive, often described as an electric shock sensation that follows the nerve pathway rather than remaining localized to one area.
Understanding Arthritis in the Spine
Arthritis encompasses over 100 different conditions that cause joint inflammation and pain. When arthritis affects the spine, it primarily targets the facet joints that connect the vertebrae, leading to inflammation, stiffness, and reduced mobility.
The most common types of spinal arthritis include osteoarthritis, which develops due to wear and tear on joint cartilage, and rheumatoid arthritis, an autoimmune condition that attacks joint tissue. Osteoarthritis typically affects older adults, while rheumatoid arthritis can occur at any age.
Spinal arthritis pain tends to be more constant and aching compared to the sharp, shooting nature of sciatica. The discomfort often worsens with movement and improves with rest, particularly in the morning when joints are stiff from inactivity.
How Arthritis Can Trigger Sciatica
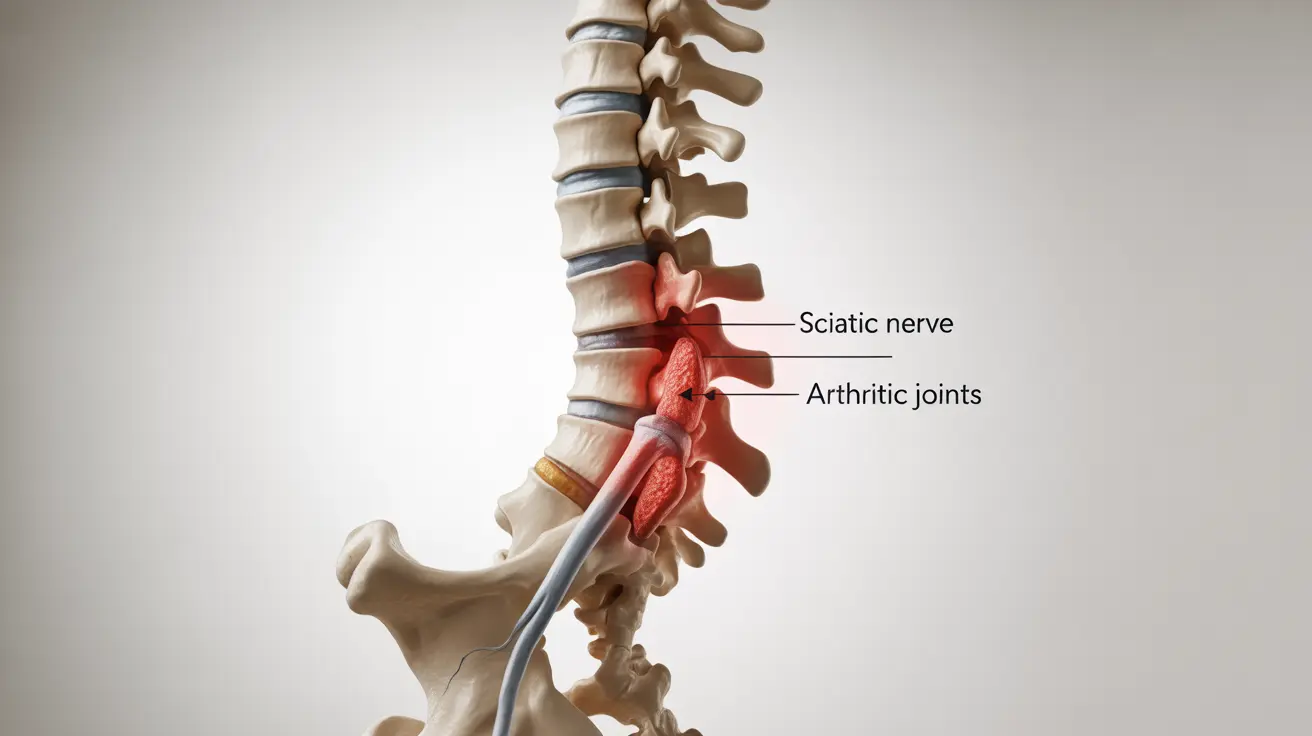
The relationship between arthritis and sciatica becomes complex when spinal arthritis creates conditions that compress the sciatic nerve. As arthritis progresses, it can lead to the formation of bone spurs, joint enlargement, and ligament thickening, all of which can narrow the spinal canal.
This narrowing, known as spinal stenosis, can put pressure on nerve roots, including those that form the sciatic nerve. When arthritis-related changes compress these nerve roots, patients may experience both arthritic joint pain and sciatic nerve pain simultaneously.
Additionally, chronic inflammation from arthritis can affect surrounding tissues, potentially contributing to muscle tension and additional pressure on the sciatic nerve. This interconnected relationship explains why some individuals experience both conditions concurrently.
Identifying Your Type of Back Pain
Distinguishing between arthritis and sciatica pain requires careful attention to specific characteristics and patterns. Sciatica typically presents as sharp, burning, or electric-like pain that travels down the leg, often accompanied by numbness or tingling in the foot or toes.
Arthritis pain, conversely, tends to be deeper, more constant, and localized to the affected joints in the spine. This pain often feels stiff and achy, particularly noticeable when getting up after sitting for extended periods or first thing in the morning.
The timing and triggers of pain can also provide important clues. Sciatica pain may worsen with certain movements like coughing, sneezing, or sitting, while arthritis pain typically increases with activity and improves with rest. Weather changes may also affect arthritis symptoms more significantly than sciatica.
Treatment Strategies for Arthritis-Related Sciatica
When arthritis contributes to sciatica, treatment approaches must address both the underlying joint inflammation and nerve compression. Conservative treatments often form the first line of defense, including anti-inflammatory medications to reduce swelling in both the joints and surrounding tissues.
Physical therapy plays a crucial role in managing both conditions by strengthening supporting muscles, improving flexibility, and teaching proper body mechanics. Specific exercises can help decompress the spine while maintaining joint mobility affected by arthritis.
Heat and cold therapy can provide relief for both conditions, with heat helping to reduce joint stiffness from arthritis and cold potentially reducing inflammation around compressed nerves. Many patients find alternating between heat and cold applications most effective.
Advanced Treatment Options
For severe cases where conservative treatments prove insufficient, more advanced interventions may be necessary. Epidural steroid injections can provide targeted relief by reducing inflammation around compressed nerve roots while potentially addressing arthritis-related inflammation.
In some cases, surgical intervention may be recommended to address structural problems causing nerve compression. Procedures might include removing bone spurs, widening the spinal canal, or stabilizing affected vertebrae, depending on the specific underlying causes.
Lifestyle Modifications and Prevention
Managing both arthritis and sciatica often requires comprehensive lifestyle adjustments. Maintaining a healthy weight reduces stress on spinal joints, potentially slowing arthritis progression while decreasing pressure on the sciatic nerve.
Regular low-impact exercise, such as swimming, walking, or cycling, can help maintain joint flexibility and muscle strength without exacerbating symptoms. Proper ergonomics at work and home, including supportive seating and correct lifting techniques, can prevent additional strain on the spine.
Stress management techniques, including meditation and relaxation exercises, may help reduce muscle tension and improve pain tolerance. Quality sleep is also essential, as poor rest can increase pain sensitivity and inflammation levels.
Frequently Asked Questions
What are the main differences between arthritis and sciatica pain?
Arthritis pain typically presents as a deep, aching sensation localized to the affected joints in the spine, often accompanied by stiffness and reduced mobility. Sciatica pain, on the other hand, is characterized by sharp, shooting, or burning sensations that travel along the sciatic nerve path from the lower back down through the leg, often reaching the foot.
Can arthritis in the spine cause sciatica symptoms?
Yes, spinal arthritis can definitely cause sciatica symptoms. As arthritis progresses, it can lead to bone spur formation, joint enlargement, and spinal canal narrowing (stenosis), which can compress the sciatic nerve roots. This compression results in the characteristic radiating pain, numbness, and tingling associated with sciatica.
How do you know if your back pain is from arthritis or sciatica?
The key is to observe pain patterns and characteristics. Sciatica typically causes sharp, electric-like pain that travels down one leg, often accompanied by numbness or tingling. Arthritis pain is usually deeper, more constant, and localized to the spine, with stiffness being particularly noticeable in the morning or after periods of inactivity. Professional medical evaluation is essential for accurate diagnosis.
What are the best treatments for sciatica caused by arthritis?
Treatment approaches should address both conditions simultaneously. Anti-inflammatory medications help reduce joint inflammation and nerve irritation. Physical therapy focusing on spinal decompression and joint mobility is crucial. Heat therapy can ease arthritis stiffness while cold therapy may reduce nerve inflammation. In severe cases, epidural injections or surgical interventions may be necessary to address structural problems.
When should you see a doctor for back pain related to arthritis or sciatica?
Seek medical attention immediately if you experience severe pain that doesn't improve with rest, progressive weakness in your legs, loss of bladder or bowel control, or numbness in the saddle area. Also consult a healthcare provider if your pain significantly interferes with daily activities, persists for more than a few weeks, or is accompanied by fever or unexplained weight loss.