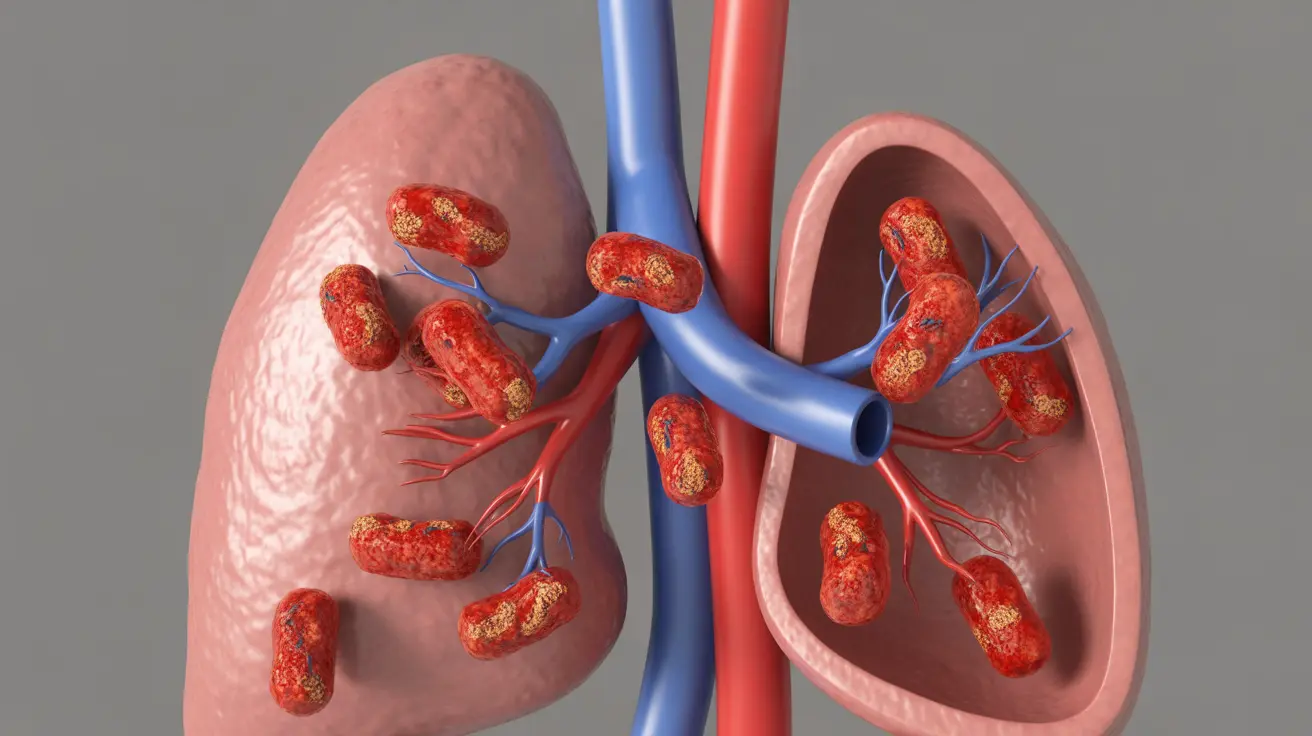
Septic emboli are serious medical conditions that occur when infected blood clots travel through the bloodstream and lodge in different organs or tissues. These dangerous emboli can spread infection throughout the body and potentially cause severe complications if not promptly identified and treated. Understanding the symptoms, risks, and treatment options is crucial for better health outcomes.
What Are Septic Emboli?
Septic emboli develop when bacteria or other infectious organisms attach to blood clots that subsequently break free and travel through the bloodstream. These infected clots can potentially damage any organ they reach, leading to various complications depending on where they settle.
Common Symptoms and Warning Signs
The symptoms of septic emboli can vary significantly depending on which organs are affected. Recognition of these symptoms is crucial for early intervention and treatment.
General Symptoms
Common systemic symptoms include:
- Fever and chills
- Fatigue and weakness
- Body aches
- Shortness of breath
- Rapid heart rate
- Confusion or altered mental state
Organ-Specific Symptoms
Different organs affected by septic emboli present distinct symptoms:
Lungs
- Chest pain
- Coughing, sometimes with blood
- Difficulty breathing
- Rapid breathing
Brain
- Severe headaches
- Vision changes
- Confusion
- Speech difficulties
- Weakness on one side of the body
Skin and Extremities
- Red, tender spots
- Small, dark lesions
- Pain and swelling
- Decreased circulation in affected areas
Risk Factors and Causes
Several conditions and circumstances can increase the risk of developing septic emboli:
- Intravenous drug use
- Heart valve infections (endocarditis)
- Recent surgical procedures
- Presence of medical devices or catheters
- Weakened immune system
- Dental infections
- Deep tissue infections
Diagnosis Methods
Healthcare providers use various diagnostic tools to identify septic emboli and their source:
- Blood cultures to identify infectious organisms
- Imaging studies (CT scans, MRI, echocardiogram)
- Physical examination
- Medical history review
- Specialized heart testing if endocarditis is suspected
Treatment Approaches
Treatment for septic emboli typically requires a comprehensive approach:
Immediate Interventions
- Intravenous antibiotics
- Supportive care
- Blood pressure management
- Oxygen therapy if needed
Long-term Management
- Extended antibiotic courses
- Treatment of underlying conditions
- Regular monitoring
- Prevention of future episodes
Prevention Strategies
Several measures can help reduce the risk of developing septic emboli:
- Proper dental hygiene
- Prompt treatment of infections
- Regular medical check-ups
- Careful management of medical devices
- Following prescribed antibiotic regimens
- Avoiding intravenous drug use
Frequently Asked Questions
What are the most common symptoms of septic emboli and how do they vary by the affected organ? Symptoms vary by location but commonly include fever, chest pain, and breathing difficulties for lung involvement; headaches and confusion for brain involvement; and skin lesions or pain for extremity involvement.
How is septic emboli diagnosed and what tests are typically done to identify the source and location? Diagnosis involves blood cultures, imaging studies like CT scans or MRI, physical examination, and often cardiac testing such as echocardiograms to identify the source and extent of infection.
What causes septic emboli and which risk factors make someone more likely to develop them? Common causes include endocarditis, intravenous drug use, and presence of medical devices. Risk factors include weakened immune system, recent surgery, and underlying infections.
How are septic emboli treated and what are the options to manage infection and complications? Treatment typically involves intensive antibiotic therapy, supportive care, and management of underlying conditions. Some cases may require surgical intervention to remove infected material or repair damaged tissues.
Can septic emboli be prevented, and what lifestyle or medical steps reduce the risk of developing them? Prevention strategies include maintaining good dental hygiene, promptly treating infections, following medical advice regarding antibiotics, and avoiding risk factors like intravenous drug use. Regular medical check-ups and proper management of medical devices are also important.