Chemotherapy plays a vital role in cancer treatment, but it's important to be aware of its potential effects on heart health. Understanding the signs of heart damage from chemo can help patients and healthcare providers monitor and address cardiac complications early, leading to better outcomes during cancer treatment.
This comprehensive guide explores the key indicators of chemotherapy-related heart problems, risk factors, monitoring methods, and available treatments to help patients navigate this aspect of their cancer journey safely.
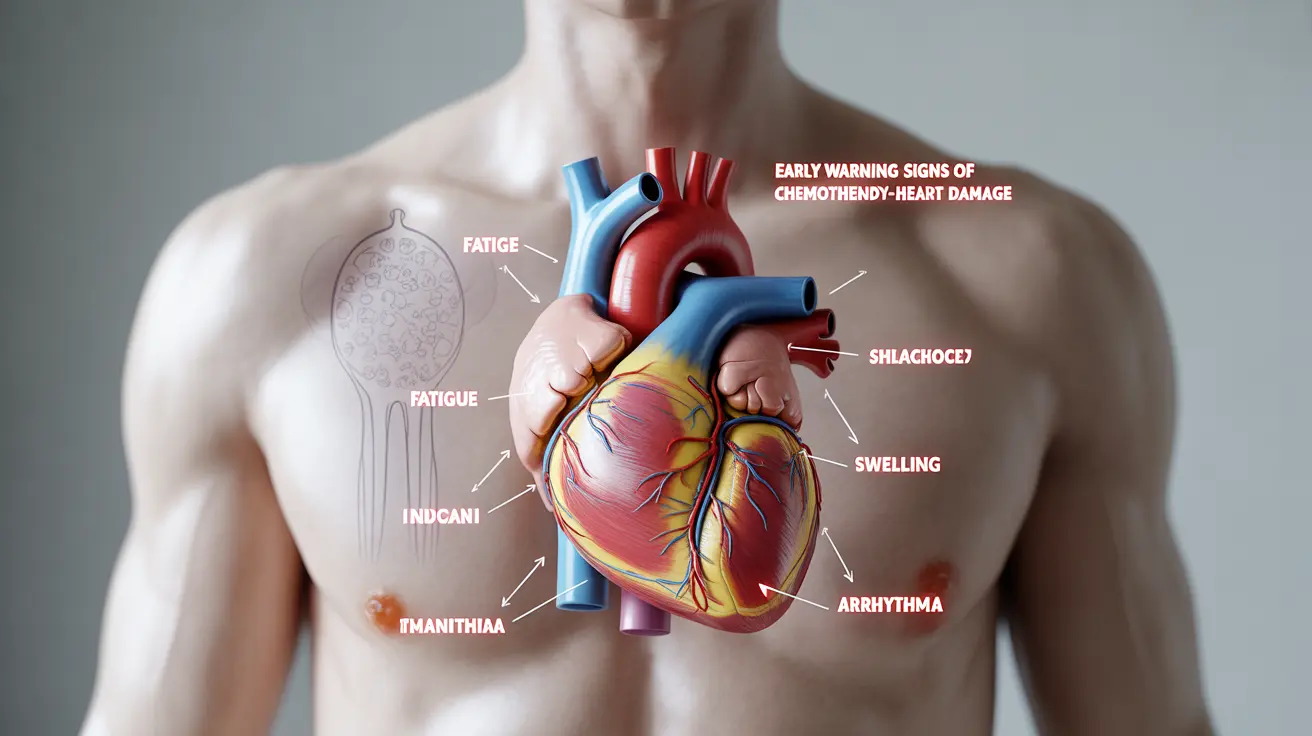
Early Warning Signs of Heart Damage During Chemotherapy
Recognizing early signs of heart damage is crucial for prompt intervention. Common indicators include:
- Unusual fatigue or weakness
- Shortness of breath, especially during mild activity
- Irregular heartbeat or heart palpitations
- Chest pain or pressure
- Swelling in the ankles, feet, or legs
- Dizziness or lightheadedness
- Rapid weight gain due to fluid retention
These symptoms may develop gradually during or after chemotherapy treatment. It's essential to report any new or worsening symptoms to your healthcare team immediately.
High-Risk Chemotherapy Medications
Certain chemotherapy drugs are known to have a higher potential for causing heart problems. The most common include:
- Anthracyclines (such as doxorubicin and epirubicin)
- Trastuzumab (Herceptin)
- Fluoropyrimidines (like 5-fluorouracil)
- Cyclophosphamide
- Taxanes
Your oncology team will carefully consider these risks when developing your treatment plan, taking into account your existing cardiac health and other risk factors.
Monitoring Heart Health During Treatment
Diagnostic Tests and Procedures
Healthcare providers use various methods to monitor heart function during chemotherapy:
- Echocardiograms
- Electrocardiograms (ECG/EKG)
- Blood tests for cardiac biomarkers
- MUGA scans
- Cardiac MRI when needed
Regular monitoring helps detect changes in heart function before serious complications develop, allowing for timely adjustments to treatment plans.
Treatment Options for Chemotherapy-Related Heart Damage
If heart damage is detected, several treatment approaches may be considered:
- Medication adjustments or temporary pause in chemotherapy
- Heart medications (ACE inhibitors, beta-blockers)
- Lifestyle modifications
- Cardiac rehabilitation programs
- Regular cardiology follow-up
The specific treatment plan will depend on the severity of heart damage and the patient's overall health status.
Prevention and Risk Reduction Strategies
Several approaches can help minimize the risk of heart damage during chemotherapy:
- Comprehensive cardiac evaluation before starting treatment
- Use of cardioprotective medications when appropriate
- Regular exercise as tolerated
- Heart-healthy diet
- Stress management
- Avoiding tobacco and limiting alcohol
- Regular monitoring of blood pressure and heart function
Frequently Asked Questions
What are the early signs of heart damage caused by chemotherapy?
Early signs include unusual fatigue, shortness of breath during mild activity, irregular heartbeat, chest discomfort, swelling in the extremities, and unexpected weight gain. These symptoms should be reported to your healthcare provider immediately.
Which chemotherapy drugs are most likely to cause heart problems?
Anthracyclines, trastuzumab, fluoropyrimidines, cyclophosphamide, and taxanes are among the chemotherapy drugs most commonly associated with heart problems. The risk varies based on dosage and individual patient factors.
How is heart damage from chemotherapy diagnosed and monitored?
Healthcare providers use regular echocardiograms, ECGs, blood tests for cardiac markers, and sometimes MUGA scans or cardiac MRI to monitor heart function during chemotherapy treatment.
What treatments are available if chemotherapy causes heart damage or heart failure?
Treatment options include adjusting chemotherapy protocols, prescribing heart medications, implementing lifestyle changes, and participating in cardiac rehabilitation programs. The approach is tailored to each patient's specific situation.
How can the risk of heart damage be reduced during chemotherapy?
Risk reduction strategies include pre-treatment cardiac evaluation, using cardioprotective medications when appropriate, maintaining regular physical activity, following a heart-healthy diet, and ongoing monitoring of heart function throughout treatment.