An intrauterine device (IUD) is a highly effective form of birth control, but like any medical device, it can occasionally lead to complications, including infections. Understanding the signs of an IUD infection is crucial for early detection and prompt treatment, helping to prevent more serious health issues from developing.
While IUD-related infections are relatively rare, especially when inserted by a qualified healthcare provider under sterile conditions, being aware of potential warning signs can help ensure quick medical intervention when needed. This comprehensive guide will help you identify infection symptoms, understand risks, and know when to seek medical attention.
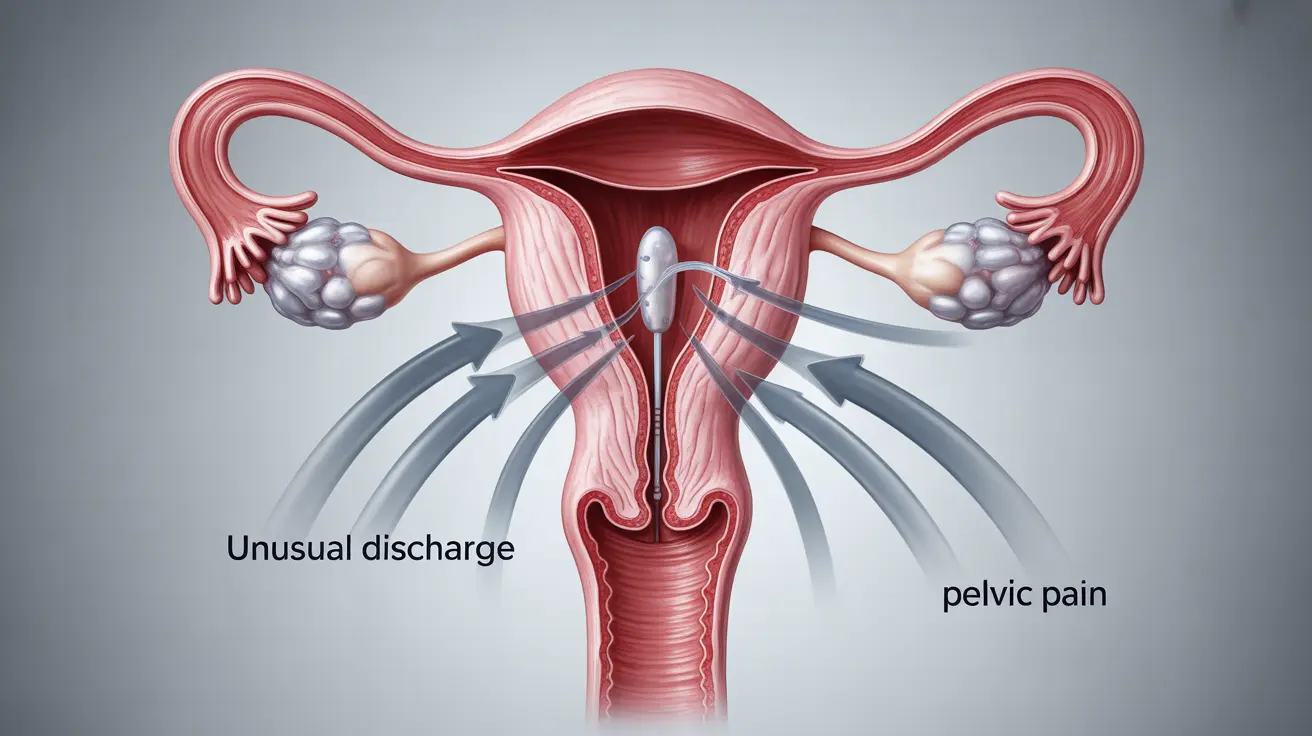
Key Signs and Symptoms of IUD Infection
Recognizing potential infection symptoms early is essential for proper treatment. Common signs include:
- Unusual vaginal discharge
- Severe pelvic or abdominal pain
- Fever and chills
- Unusual bleeding between periods
- Pain during sexual intercourse
- Strong-smelling vaginal odor
If you experience any combination of these symptoms, especially within the first few weeks after IUD insertion, it's important to contact your healthcare provider promptly.
Understanding IUD-Related Infections and PID
IUD-related infections often develop into Pelvic Inflammatory Disease (PID) if left untreated. PID is an infection of the female reproductive organs that can have serious consequences if not addressed promptly.
How Infections Develop
Infections typically occur through one of two main pathways:
- During insertion: Bacteria may enter the uterus during the IUD placement procedure
- Post-insertion: Existing vaginal bacteria may travel up the IUD strings into the uterus
When to Seek Immediate Medical Care
Certain symptoms warrant immediate medical attention:
- Severe abdominal pain that doesn't subside
- High fever (101°F or higher)
- Heavy bleeding that soaks through multiple pads per hour
- Severe pain with movement
- Symptoms that worsen over time
Diagnosis and Treatment Options
Healthcare providers typically diagnose IUD-related infections through:
- Physical examination
- Laboratory tests of vaginal discharge
- Blood tests to check for infection markers
- Ultrasound imaging if necessary
Treatment usually involves:
- Antibiotic therapy
- Pain management
- Possible IUD removal in severe cases
- Follow-up care to ensure complete recovery
Prevention Strategies
Several measures can help reduce the risk of IUD-related infections:
- Choose an experienced healthcare provider for insertion
- Follow post-insertion care instructions carefully
- Maintain good hygiene practices
- Attend all follow-up appointments
- Monitor for any unusual symptoms
Frequently Asked Questions
What are the common signs of an infection after IUD insertion?
Common signs include unusual vaginal discharge, severe pelvic pain, fever, abnormal bleeding, pain during intercourse, and strong vaginal odor. Any combination of these symptoms warrants medical attention.
How can an IUD lead to pelvic inflammatory disease (PID)?
An IUD can potentially allow bacteria to travel up into the uterus, either during insertion or afterward along the IUD strings. This bacterial migration can lead to PID if left untreated, affecting the reproductive organs.
When should I see a doctor if I suspect an IUD infection?
Seek immediate medical attention if you experience severe abdominal pain, high fever, heavy bleeding, severe pain with movement, or if your symptoms worsen over time.
How is an infection related to an IUD diagnosed and treated?
Diagnosis typically involves physical examination, laboratory tests, and possibly imaging studies. Treatment usually consists of antibiotics, pain management, and in some cases, IUD removal.
Can infections after IUD insertion be prevented and how?
While not all infections can be prevented, risks can be minimized by choosing an experienced provider, following proper aftercare instructions, maintaining good hygiene, and attending follow-up appointments.