Alcoholic pancreatitis is a serious inflammatory condition of the pancreas that develops from prolonged heavy alcohol use. Recognizing the early warning signs and symptoms is crucial for getting timely medical treatment and preventing severe complications. Understanding what to look for can help you identify this condition before it progresses to a more dangerous state.
Understanding Alcoholic Pancreatitis
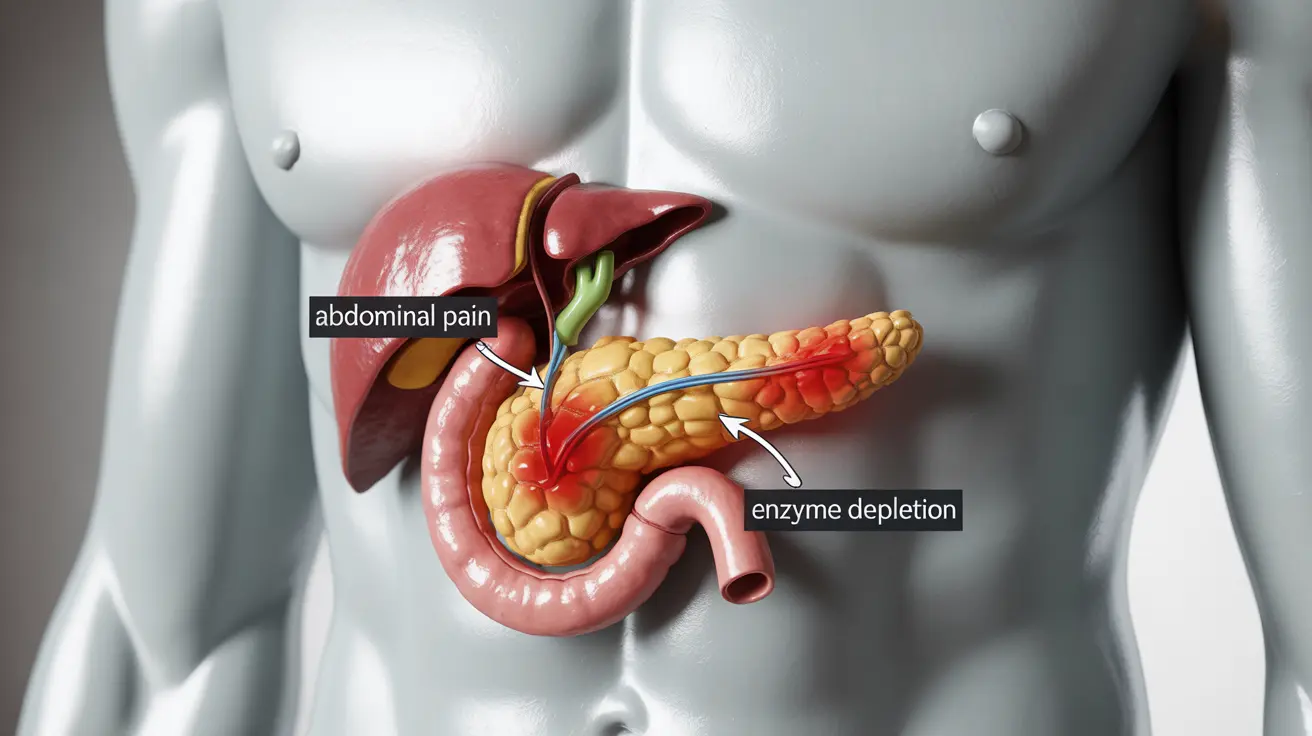
When alcohol repeatedly damages the pancreas, it can lead to inflammation and eventually cause pancreatitis. This condition can occur as either acute (sudden onset) or chronic (long-term) pancreatitis, with each form presenting distinct patterns of symptoms and potential complications.
Key Warning Signs and Symptoms
The signs of pancreatitis from alcohol consumption often develop gradually, though they can sometimes appear suddenly. Common symptoms include:
- Upper abdominal pain that may radiate to the back
- Nausea and vomiting
- Tenderness when touching the abdomen
- Fever and increased heart rate
- Unexplained weight loss
- Oily, foul-smelling stools
Characteristic Pain Patterns
The pain associated with alcoholic pancreatitis typically presents as a constant, dull ache in the upper abdomen that often becomes worse after eating. Many patients describe the pain as being more severe when lying flat on their back, finding relief by sitting forward or curling into a fetal position.
Diagnostic Process
Healthcare providers use several methods to confirm a diagnosis of alcoholic pancreatitis:
- Blood tests to measure pancreatic enzyme levels
- Imaging studies like CT scans or ultrasound
- Physical examination and medical history review
- Tests to rule out other conditions with similar symptoms
Treatment Approaches
The treatment of alcoholic pancreatitis focuses on several key areas:
- Complete cessation of alcohol consumption
- Pain management through appropriate medications
- Nutritional support and dietary modifications
- Fluid therapy to prevent dehydration
- Treatment of any complications that may develop
Lifestyle Changes and Prevention
Preventing further pancreatic damage requires significant lifestyle modifications:
- Absolute abstinence from alcohol
- Following a low-fat diet
- Regular medical check-ups
- Smoking cessation
- Staying well-hydrated
Complications and Long-term Outlook
Without proper treatment, alcoholic pancreatitis can lead to serious complications:
- Chronic pain
- Diabetes development
- Pancreatic pseudocysts
- Increased risk of pancreatic cancer
- Malnutrition and digestive problems
Frequently Asked Questions
What are the common signs and symptoms of pancreatitis caused by heavy alcohol use?
The most common signs include severe upper abdominal pain, nausea, vomiting, fever, and rapid heartbeat. Patients may also experience digestive issues and unexplained weight loss. These symptoms often worsen after eating or drinking.
How does alcoholic pancreatitis pain typically feel and where is it located?
The pain is usually felt in the upper abdomen and may radiate to the back. It's typically described as a constant, dull ache that worsens after eating and when lying flat. Many patients find relief by sitting forward or curling up.
What tests and procedures are used to diagnose pancreatitis related to alcohol consumption?
Diagnosis typically involves blood tests to check pancreatic enzyme levels, imaging studies such as CT scans or ultrasounds, and a thorough medical history. Doctors may also perform physical examinations and additional tests to rule out other conditions.
How is alcoholic pancreatitis treated and what lifestyle changes can help prevent it?
Treatment includes complete alcohol cessation, pain management, nutritional support, and fluid therapy. Prevention requires permanent abstinence from alcohol, following a low-fat diet, regular medical check-ups, and maintaining proper hydration.
What complications can develop if alcoholic pancreatitis is left untreated or becomes chronic?
Untreated alcoholic pancreatitis can lead to chronic pain, diabetes, pancreatic pseudocysts, increased cancer risk, and severe digestive problems. Long-term complications may also include malnutrition and permanent pancreatic damage.