A soft cervix, also known as cervical softening or cervical ripening, is a natural occurrence during pregnancy and ovulation. However, when cervical softening happens at unexpected times or becomes a medical concern during pregnancy, it's important to understand the implications and available treatments.
This comprehensive guide explores what causes a soft cervix, its potential risks during pregnancy, and when to seek medical attention. We'll also discuss diagnosis methods and treatment options to help manage this condition effectively.
What Is a Soft Cervix?
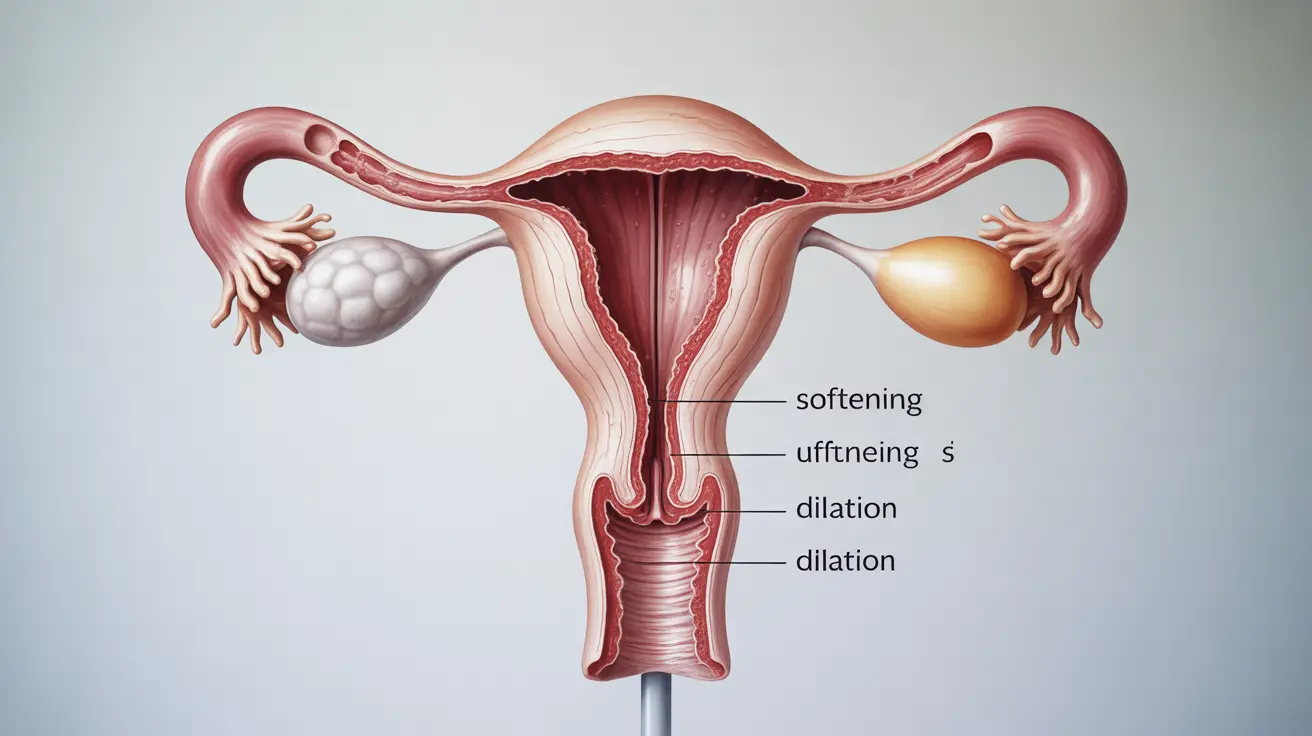
The cervix is the lower part of the uterus that connects to the vagina. During normal circumstances, the cervix maintains a firm consistency, similar to the tip of your nose. However, various factors can cause it to become softer, which may or may not indicate a medical concern.
During pregnancy, the cervix naturally softens as part of the body's preparation for childbirth. This process, known as cervical ripening, typically occurs in the final weeks of pregnancy. However, if it happens too early, it may indicate potential complications.
Causes of Cervical Softening
Natural Causes
Several natural processes can lead to cervical softening:
- Hormonal changes during the menstrual cycle
- Pregnancy progression
- Approaching labor and delivery
- Ovulation
Medical Conditions
Sometimes, cervical softening may be related to underlying conditions:
- Cervical insufficiency
- Previous cervical trauma
- Congenital uterine abnormalities
- Hormonal imbalances
Risks During Pregnancy
When cervical softening occurs too early in pregnancy, it may lead to cervical insufficiency, which can increase the risk of pregnancy complications. These risks include:
- Preterm labor
- Premature rupture of membranes
- Second-trimester pregnancy loss
- Increased risk of infection
Diagnosis and Monitoring
Healthcare providers use several methods to assess cervical health during pregnancy:
- Transvaginal ultrasound
- Physical examination
- Medical history review
- Cervical length measurement
- Fetal fibronectin testing when appropriate
Treatment Options
Treatment approaches vary depending on the underlying cause and timing of cervical softening:
Preventive Measures
- Regular prenatal check-ups
- Cervical length monitoring
- Activity modification when necessary
- Progesterone supplementation in some cases
Medical Interventions
For cases requiring medical intervention, treatments may include:
- Cervical cerclage (cervical stitch)
- Progesterone therapy
- Bed rest when indicated
- Close monitoring of pregnancy progression
Frequently Asked Questions
What does it mean if I have a soft cervix outside of ovulation or pregnancy?
A soft cervix outside of ovulation or pregnancy could be related to hormonal changes, menstrual cycle variations, or underlying medical conditions. While some cervical changes are normal, unexpected softening should be evaluated by a healthcare provider to rule out any concerns.
How can a soft cervix affect my pregnancy and risk of preterm labor?
A soft cervix during pregnancy, especially if it occurs too early, can increase the risk of preterm labor and pregnancy complications. It may lead to cervical insufficiency, which can cause the cervix to open prematurely, potentially resulting in preterm birth or pregnancy loss.
What are common causes of a cervix becoming too soft or weak during pregnancy?
Common causes include previous cervical procedures, trauma to the cervix, congenital uterine abnormalities, and hormonal factors. Some women may have an inherited predisposition to cervical weakness.
How is cervical insufficiency diagnosed and treated to prevent premature birth?
Diagnosis typically involves transvaginal ultrasound measurements of cervical length and physical examinations. Treatment options may include cervical cerclage, progesterone therapy, and close monitoring throughout pregnancy.
When should I see a doctor if I notice my cervix feels softer or different than usual?
Contact your healthcare provider if you notice any unusual changes in your cervix, experience unexpected vaginal discharge, pelvic pressure, or discomfort. During pregnancy, report any symptoms immediately, particularly if you have a history of cervical insufficiency or preterm labor.