Spongiotic dermatitis is a common inflammatory skin condition that affects millions of people worldwide, causing uncomfortable symptoms like itching, redness, and swelling. This skin disorder gets its name from the characteristic "spongy" appearance of affected tissue when examined under a microscope, where fluid accumulates between skin cells in the upper layer of the epidermis.
While the term might sound complex, spongiotic dermatitis actually encompasses several familiar skin conditions, including eczema, contact dermatitis, and atopic dermatitis. Understanding this condition is crucial for anyone experiencing persistent skin irritation, as proper identification and treatment can significantly improve quality of life and prevent complications.
What Causes Spongiotic Dermatitis?
Spongiotic dermatitis develops through a complex interplay of genetic predisposition, environmental factors, and immune system responses. The condition occurs when the skin's barrier function becomes compromised, allowing irritants and allergens to penetrate more easily and trigger inflammatory reactions.
Genetic factors play a significant role, particularly in atopic dermatitis, where family history of allergies, asthma, or eczema increases the likelihood of developing the condition. Individuals with certain genetic variations affecting skin barrier proteins, such as filaggrin mutations, are more susceptible to developing spongiotic dermatitis.
Environmental triggers are equally important in the development and progression of this skin condition. Common external factors include exposure to harsh chemicals, fragrances, detergents, and certain metals like nickel. Weather conditions, particularly cold, dry air or excessive humidity, can also exacerbate symptoms by disrupting the skin's natural moisture balance.
Recognizing the Symptoms
The hallmark symptoms of spongiotic dermatitis typically begin with intense itching, which often precedes visible skin changes. This pruritus can be particularly troublesome at night, disrupting sleep patterns and affecting daily activities. The itching sensation may range from mild discomfort to severe, uncontrollable urges to scratch.
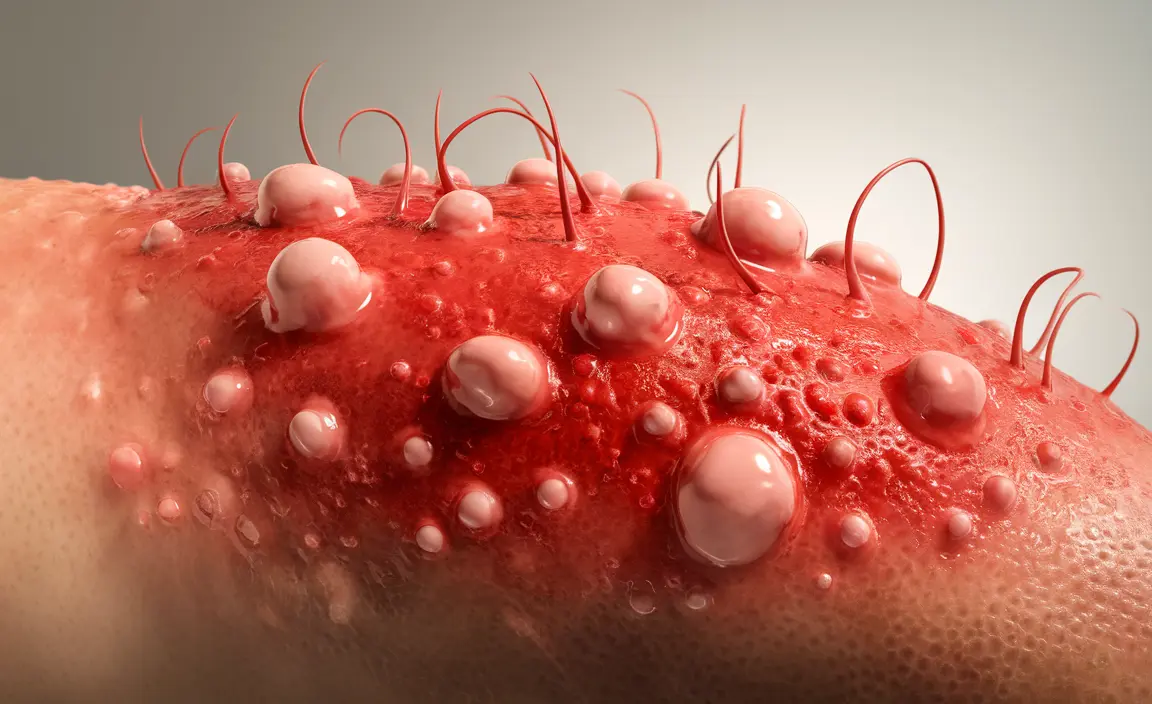
Visual symptoms develop as the condition progresses, starting with redness and inflammation in affected areas. The skin may appear swollen due to fluid accumulation, giving it a puffy or thickened appearance. In acute phases, small fluid-filled blisters or vesicles may form, which can burst and weep clear fluid, leading to crusting and scaling.
Chronic cases of spongiotic dermatitis often present with different characteristics. The affected skin becomes thickened and leathery through a process called lichenification, which results from repeated scratching and rubbing. The skin may develop a darker pigmentation and exhibit more pronounced scaling and dryness.
Professional Diagnosis Process
Diagnosing spongiotic dermatitis requires a comprehensive approach that combines clinical examination with detailed patient history. Dermatologists begin by conducting a thorough visual inspection of the affected areas, noting the distribution pattern, appearance, and severity of symptoms.
The diagnostic process includes a detailed discussion of the patient's medical history, family history of skin conditions, and potential exposure to irritants or allergens. Healthcare providers pay particular attention to the timeline of symptom development, identifying possible triggers, and assessing the impact on the patient's quality of life.
In many cases, a skin biopsy may be necessary to confirm the diagnosis and rule out other skin conditions. The biopsy reveals the characteristic spongiosis – the accumulation of fluid between skin cells – that gives this condition its name. Additionally, patch testing might be recommended to identify specific allergens that could be triggering contact dermatitis reactions.
Treatment Approaches and Management
Effective treatment of spongiotic dermatitis typically involves a multi-faceted approach that addresses both immediate symptom relief and long-term management. The primary goals include reducing inflammation, controlling itching, restoring skin barrier function, and preventing secondary infections.
Topical corticosteroids remain the gold standard for treating acute flare-ups of spongiotic dermatitis. These medications effectively reduce inflammation and provide rapid relief from itching and redness. However, their use must be carefully monitored to avoid potential side effects, particularly with long-term application.
Non-steroidal topical treatments offer valuable alternatives for long-term management. Calcineurin inhibitors, such as tacrolimus and pimecrolimus, provide effective anti-inflammatory action without the side effects associated with prolonged steroid use. These medications are particularly useful for treating sensitive areas like the face and eyelids.
Moisturization plays a crucial role in managing spongiotic dermatitis by restoring and maintaining the skin barrier function. Regular application of fragrance-free, hypoallergenic moisturizers helps prevent water loss and reduces the penetration of irritants and allergens. The timing of moisturizer application is important – it should be applied to slightly damp skin to lock in moisture effectively.
Prevention Strategies and Lifestyle Modifications
Preventing flare-ups of spongiotic dermatitis requires a proactive approach that focuses on identifying and avoiding triggers while maintaining optimal skin health. The foundation of prevention lies in establishing a gentle, consistent skincare routine that supports the skin's natural barrier function.
Environmental modifications can significantly reduce the frequency and severity of flare-ups. This includes maintaining appropriate humidity levels in living spaces, using air purifiers to reduce airborne allergens, and choosing clothing made from soft, breathable fabrics like cotton. Avoiding known irritants and allergens is equally important, which may require reading product labels carefully and choosing hypoallergenic alternatives.
Stress management techniques can also play a valuable role in preventing flare-ups, as psychological stress is known to exacerbate inflammatory skin conditions. Regular exercise, adequate sleep, and relaxation techniques such as meditation or yoga may help reduce stress-related triggers.
Dietary considerations, while not universally applicable, may benefit some individuals with spongiotic dermatitis. Identifying and avoiding food triggers through elimination diets, when appropriate, can help reduce systemic inflammation that may contribute to skin symptoms.
Frequently Asked Questions
What are the common causes and triggers of spongiotic dermatitis?
Spongiotic dermatitis develops from a combination of genetic predisposition and environmental triggers. Common causes include exposure to irritants like harsh soaps, detergents, and chemicals, as well as allergens such as fragrances, metals, and certain fabrics. Weather conditions, stress, hormonal changes, and certain foods can also trigger flare-ups in susceptible individuals.
What symptoms should I look for to identify spongiotic dermatitis?
The primary symptoms include intense itching, redness, and swelling of the affected skin. You may notice small fluid-filled blisters, weeping or crusting areas, and scaling or flaking skin. In chronic cases, the skin may become thickened, leathery, and darker in color due to repeated scratching and inflammation.
How is spongiotic dermatitis diagnosed by a doctor or dermatologist?
Diagnosis involves a comprehensive clinical examination combined with detailed medical history review. Your dermatologist will assess the appearance and distribution of skin lesions, discuss potential triggers and family history, and may perform additional tests such as skin biopsies or patch testing to confirm the diagnosis and identify specific allergens.
What are the most effective treatments and home care options for managing spongiotic dermatitis?
Treatment typically includes topical corticosteroids for acute flare-ups, non-steroidal anti-inflammatory creams for long-term use, and consistent moisturization with fragrance-free products. Home care involves gentle cleansing with mild soaps, avoiding hot water, applying cool compresses during flare-ups, and maintaining proper humidity levels in your environment.
How can I prevent flare-ups and reduce the risk of spongiotic dermatitis worsening?
Prevention strategies include identifying and avoiding personal triggers, maintaining a gentle skincare routine with hypoallergenic products, wearing soft fabrics, managing stress levels, and keeping the skin well-moisturized. Environmental modifications such as using air purifiers, maintaining appropriate humidity, and avoiding extreme temperatures can also help prevent flare-ups.