Diabetes is a complex metabolic disorder that develops and progresses through distinct stages. Understanding these stages is crucial for early detection, prevention, and effective management of both type 1 and type 2 diabetes. This comprehensive guide will explore the progression of diabetes, helping you recognize important signs and take appropriate action at each stage.
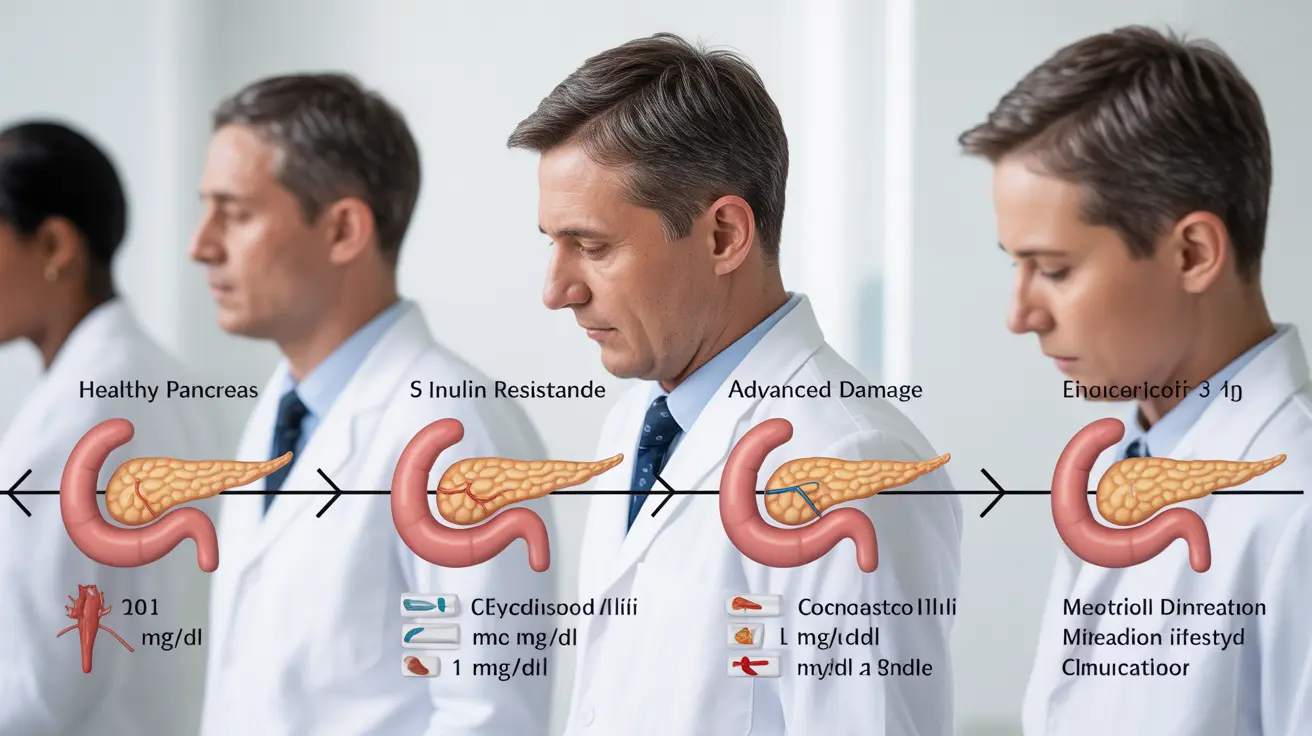
The Progressive Nature of Diabetes
Both type 1 and type 2 diabetes follow different developmental patterns, with distinct characteristics and intervention opportunities at each stage. Recognizing these stages early can significantly impact treatment outcomes and quality of life.
Stages of Type 1 Diabetes
Stage 1: Early Autoimmune Response
During this initial stage, the immune system begins attacking insulin-producing beta cells in the pancreas. Blood tests may show diabetes-related autoantibodies, but blood sugar levels typically remain normal. No obvious symptoms are present at this point.
Stage 2: Beta Cell Decline
As more beta cells are destroyed, subtle blood sugar abnormalities begin to appear. While obvious symptoms may still be absent, glucose tolerance tests might show irregular results. This stage presents a crucial window for early intervention.
Stage 3: Clinical Diagnosis
By this stage, significant beta cell loss has occurred, leading to classic diabetes symptoms such as:
- Increased thirst and urination
- Unexplained weight loss
- Extreme fatigue
- Blurred vision
Stages of Type 2 Diabetes
Stage 1: Insulin Resistance
The body's cells begin showing reduced sensitivity to insulin, though blood sugar levels may still be normal. Risk factors like obesity, sedentary lifestyle, and family history often contribute to this stage.
Stage 2: Prediabetes
Blood sugar levels become elevated but haven't reached diabetic thresholds. This crucial stage offers an important opportunity for lifestyle interventions to prevent or delay progression to full diabetes.
Stage 3: Early Type 2 Diabetes
Blood glucose levels consistently exceed normal ranges, leading to an official diabetes diagnosis. Some people may experience mild symptoms, while others might not notice any changes.
Stage 4: Established Type 2 Diabetes
Without proper management, this stage can involve complications and may require multiple medications. Consistent monitoring and adherence to treatment become essential.
Early Detection and Prevention
Regular screening is vital for those with risk factors. Early intervention strategies include:
- Regular physical activity
- Balanced, nutrient-rich diet
- Weight management
- Blood sugar monitoring
- Stress management
- Regular medical check-ups
Treatment Approaches by Stage
Treatment strategies vary depending on the type and stage of diabetes. Early stages often focus on lifestyle modifications, while later stages may require medication or insulin therapy. Working closely with healthcare providers ensures appropriate treatment adjustments as the condition progresses.
Frequently Asked Questions
What are the different stages of type 1 and type 2 diabetes and how do they affect blood sugar levels?
Type 1 diabetes progresses through three main stages: early autoimmune response, beta cell decline, and clinical diagnosis. Type 2 diabetes develops through insulin resistance, prediabetes, early diabetes, and established diabetes. Each stage shows increasingly abnormal blood sugar levels as the condition progresses.
How can knowing the stages of diabetes help in early diagnosis and prevention of complications?
Understanding diabetes stages enables early intervention, allowing for lifestyle changes or medical treatments that can slow or prevent disease progression. This knowledge helps individuals and healthcare providers monitor risk factors and implement appropriate interventions at the most effective times.
What symptoms should I expect to see at each stage of type 1 and type 2 diabetes?
Early stages of both types may show few or no symptoms. As type 1 progresses, symptoms like increased thirst, frequent urination, and weight loss appear suddenly. Type 2 symptoms develop gradually and may include fatigue, blurred vision, slow-healing wounds, and increased hunger.
How is insulin resistance related to the progression of type 2 diabetes stages?
Insulin resistance is the initial stage of type 2 diabetes, where cells become less responsive to insulin. This resistance leads to increased insulin production and eventually, if untreated, to prediabetes and full diabetes as the pancreas struggles to maintain normal blood sugar levels.
What lifestyle changes and treatments are recommended for managing diabetes at the early stages?
Early management focuses on regular exercise, healthy eating habits, weight control, and stress management. For type 2 diabetes, these lifestyle changes may prevent or delay progression. Type 1 diabetes requires insulin therapy upon diagnosis, along with lifestyle management strategies.