When someone experiences a heart attack, quick and effective treatment is crucial for survival and recovery. One of the most common interventional procedures performed after a heart attack is stent placement, which helps restore blood flow to the heart and prevents future blockages. This comprehensive guide will explain everything you need to know about getting a stent after a heart attack.
What Is a Stent and Why Is It Needed?
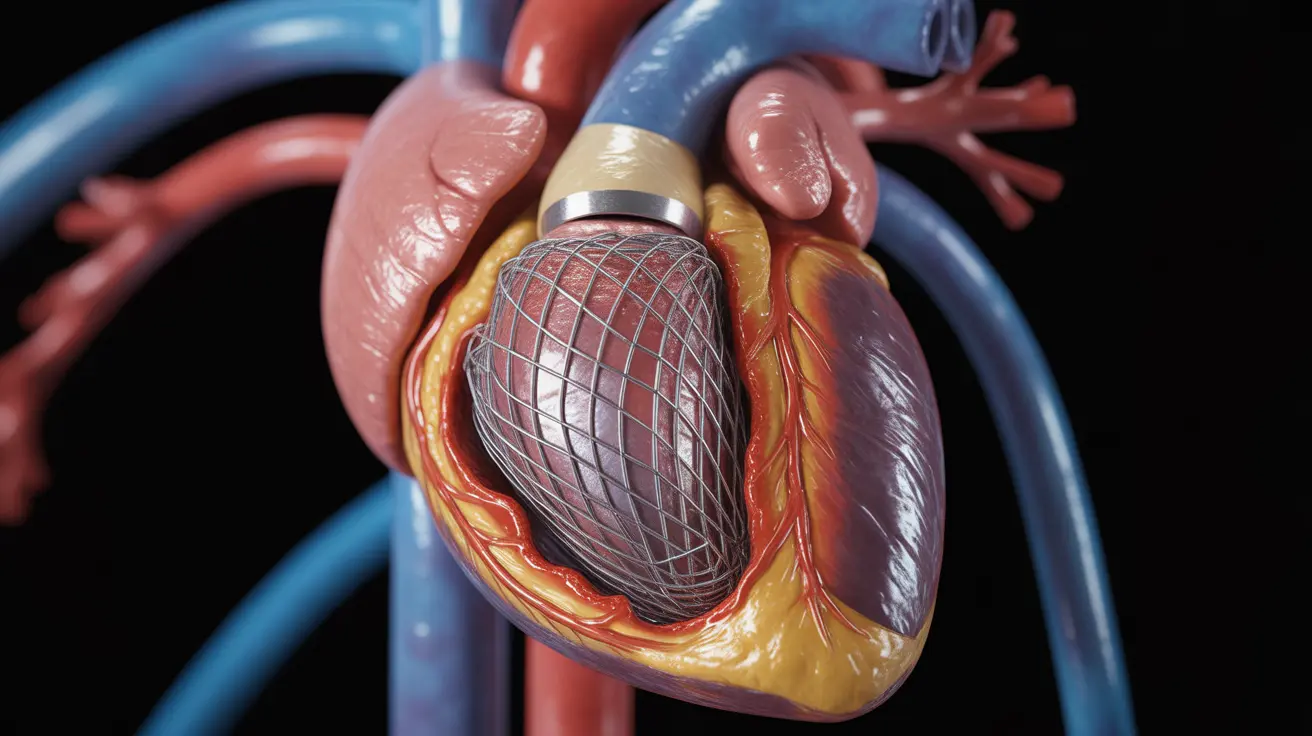
A stent is a tiny, mesh-like tube that doctors insert into a blocked or narrowed artery to keep it open. After a heart attack, which occurs when blood flow to the heart is severely restricted or blocked, a stent serves as a crucial support structure to maintain proper blood flow and prevent future cardiac events.
The Stent Placement Procedure
During the procedure, known as angioplasty with stent placement, doctors thread a thin catheter through a blood vessel, typically starting in the groin or wrist. Using X-ray guidance, they position the catheter at the blockage site. The stent, mounted on a tiny balloon, is then expanded to push back the plaque and hold the artery open.
Types of Stents Used After Heart Attacks
There are two main types of stents used in cardiac procedures:
- Bare-metal stents (BMS)
- Drug-eluting stents (DES)
Each type has specific advantages and is chosen based on individual patient factors and medical history.
Recovery Timeline After Stent Placement
Recovery after receiving a stent varies from person to person but typically follows this general timeline:
- Initial hospital stay: 2-3 days
- Limited physical activity: 1 week
- Return to normal activities: 2-4 weeks
- Complete recovery: 4-6 weeks
During this time, patients must carefully follow their doctor's instructions and attend all follow-up appointments.
Managing Life After Stent Placement
Required Medications
After receiving a stent, patients typically need to take several medications:
- Antiplatelet medications
- Blood thinners
- Statins
- Blood pressure medications
Essential Lifestyle Changes
Long-term success after stent placement requires significant lifestyle modifications:
- Maintaining a heart-healthy diet
- Regular exercise as approved by your doctor
- Smoking cessation
- Stress management
- Blood pressure monitoring
Potential Risks and Complications
While stent placement is generally safe and effective, patients should be aware of possible complications:
- Bleeding at the insertion site
- Blood clots
- Restenosis (re-narrowing of the artery)
- Allergic reactions to medications or dye
- Infection
Frequently Asked Questions
What is the purpose of placing a stent after a heart attack? A stent helps keep the affected artery open after a heart attack, restoring proper blood flow to the heart muscle and preventing future blockages. It serves as a permanent scaffold to maintain vessel patency and reduce the risk of another cardiac event.
How long does it take to recover after getting a stent following a heart attack? Most patients spend 2-3 days in the hospital and can return to normal activities within 2-4 weeks. Complete recovery typically takes 4-6 weeks, though this varies based on individual circumstances and overall health.
What are the risks and possible complications of having a stent placed after a heart attack? Common risks include bleeding, blood clots, restenosis (artery re-narrowing), allergic reactions, and infection. While these complications are possible, the benefits of stent placement usually outweigh the risks for heart attack patients.
What lifestyle changes and medications are needed after stent placement to prevent future heart problems? Patients must take prescribed medications (including antiplatelets and blood thinners), maintain a heart-healthy diet, exercise regularly as approved by their doctor, quit smoking, manage stress, and monitor their blood pressure regularly.
How does a drug-eluting stent differ from a regular stent and what are its benefits? Drug-eluting stents are coated with medication that is slowly released into the artery wall. This medication helps prevent scar tissue formation and reduces the risk of restenosis compared to bare-metal stents. They are particularly beneficial for patients at higher risk of arterial re-narrowing.