Subclinical hypothyroidism represents a subtle form of thyroid dysfunction that affects millions of people worldwide, yet many remain unaware of their condition. Unlike overt hypothyroidism, this condition presents with mildly elevated thyroid-stimulating hormone (TSH) levels while thyroid hormone levels remain within normal ranges, creating a complex diagnostic and treatment landscape.
This mild thyroid disorder can significantly impact your quality of life and long-term health, making it essential to understand its symptoms, causes, and treatment options. Early recognition and appropriate management can prevent progression to more severe thyroid dysfunction and reduce associated health risks.
What Is Subclinical Hypothyroidism?
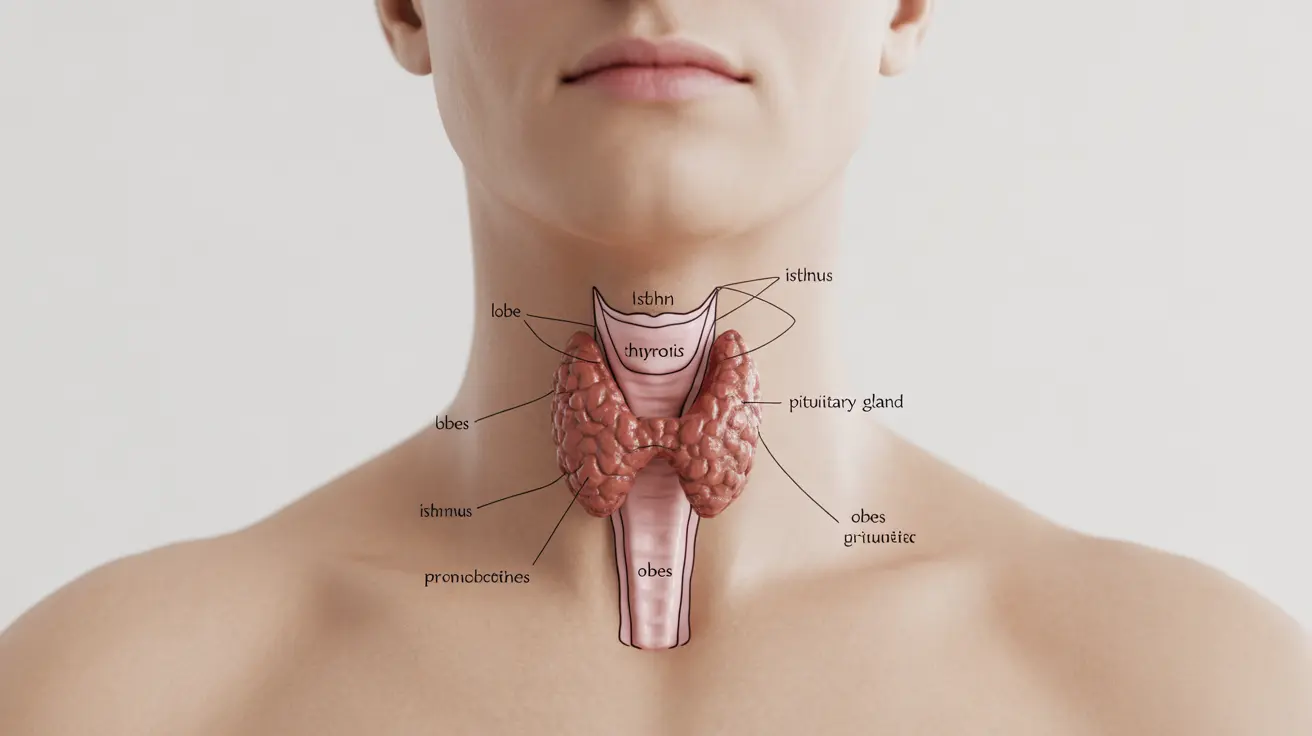
Subclinical hypothyroidism occurs when your thyroid gland produces slightly less hormone than your body needs, causing your pituitary gland to release more thyroid-stimulating hormone (TSH) to compensate. Laboratory tests typically show elevated TSH levels (usually between 4.5 and 10 mIU/L) while free thyroxine (T4) and triiodothyronine (T3) levels remain within the normal reference range.
This condition represents an intermediate state between normal thyroid function and overt hypothyroidism. The "subclinical" designation means that symptoms may be absent or very mild, making the condition difficult to detect without blood testing. However, even these subtle changes in thyroid function can affect various body systems and overall well-being.
Recognizing the Symptoms
The symptoms of subclinical hypothyroidism can be subtle and nonspecific, often mistaken for signs of aging, stress, or other health conditions. Many individuals experience fatigue that doesn't improve with rest, making daily activities feel more challenging than usual.
Common symptoms include persistent tiredness, mild weight gain that's difficult to explain, increased sensitivity to cold temperatures, and subtle changes in mood such as mild depression or irritability. Some people notice their hair becoming thinner or more brittle, while others experience dry skin or constipation.
Cognitive symptoms may also occur, including difficulty concentrating, mild memory problems, or feeling mentally "foggy." These symptoms often develop gradually, making them easy to overlook or attribute to other factors like busy lifestyles or natural aging processes.
Understanding the Causes and Risk Factors
Autoimmune thyroiditis, particularly Hashimoto's thyroiditis, represents the most common cause of subclinical hypothyroidism in areas with sufficient iodine intake. This condition occurs when the immune system mistakenly attacks thyroid tissue, gradually reducing the gland's ability to produce adequate hormones.
Previous thyroid surgery, radioactive iodine treatment, or external radiation therapy to the neck area can damage thyroid tissue and lead to subclinical hypothyroidism. Certain medications, including lithium, amiodarone, and some immunotherapy drugs, may also interfere with thyroid function.
Several factors increase the risk of developing this condition. Women face a significantly higher risk than men, particularly those over 60 years of age. Having a family history of thyroid disease, type 1 diabetes, or other autoimmune conditions also elevates risk. Pregnancy and the postpartum period represent times of increased vulnerability to thyroid dysfunction.
Diagnostic Process and Blood Tests
Diagnosing subclinical hypothyroidism requires specific blood tests that measure thyroid function markers. The primary screening test measures TSH levels, which become elevated when the thyroid gland isn't producing sufficient hormones to meet the body's needs.
Healthcare providers typically order additional tests including free T4 and sometimes free T3 levels to confirm the diagnosis. In subclinical hypothyroidism, TSH levels are elevated (usually above 4.5 mIU/L) while T4 and T3 levels remain within the normal reference range. This combination distinguishes subclinical from overt hypothyroidism.
Testing for thyroid peroxidase (TPO) antibodies helps identify autoimmune causes, particularly Hashimoto's thyroiditis. Elevated antibody levels suggest ongoing autoimmune activity and may influence treatment decisions. Healthcare providers often recommend repeat testing after 2-3 months to confirm persistent elevation before making treatment decisions.
Treatment Considerations and Levothyroxine Therapy
The decision to treat subclinical hypothyroidism with levothyroxine medication depends on several factors, including TSH levels, symptoms, age, and individual risk factors. Treatment guidelines vary, but most endocrinologists consider treatment when TSH levels exceed 10 mIU/L, regardless of symptoms.
For TSH levels between 4.5 and 10 mIU/L, treatment decisions become more individualized. Factors favoring treatment include the presence of symptoms consistent with hypothyroidism, positive TPO antibodies indicating autoimmune thyroiditis, pregnancy or plans to conceive, and cardiovascular risk factors.
When prescribed, levothyroxine therapy typically starts with low doses, usually 25-50 micrograms daily, with careful monitoring and dose adjustments based on follow-up blood tests. The goal is to normalize TSH levels while avoiding overtreatment that could lead to hyperthyroid symptoms.
Potential Health Complications
While subclinical hypothyroidism may seem mild, untreated cases can lead to several health complications over time. Cardiovascular effects represent one of the most concerning potential consequences, with some studies suggesting increased risk of heart disease, elevated cholesterol levels, and arterial stiffness.
The condition may contribute to cognitive decline, particularly in older adults, affecting memory, concentration, and overall mental sharpness. Mood disturbances, including depression and anxiety, may worsen over time without appropriate intervention.
Women with untreated subclinical hypothyroidism may experience menstrual irregularities and fertility problems. During pregnancy, the condition can increase risks of complications including preeclampsia, placental abruption, and premature birth. Additionally, there's potential for progression to overt hypothyroidism, particularly in individuals with positive thyroid antibodies.
Lifestyle Management and Support
While medication may be necessary for some individuals, certain lifestyle modifications can support thyroid health and overall well-being. Maintaining a balanced diet rich in iodine, selenium, and zinc supports optimal thyroid function, though supplementation should only occur under medical supervision.
Regular exercise can help combat fatigue, support metabolism, and improve mood symptoms associated with subclinical hypothyroidism. Stress management techniques, including meditation, yoga, or counseling, may help address both the physical and emotional aspects of the condition.
Ensuring adequate sleep and maintaining consistent sleep schedules supports the body's natural hormone rhythms. Some individuals benefit from avoiding foods that may interfere with thyroid function, such as excessive soy products or raw cruciferous vegetables, though moderate consumption is typically acceptable.
Frequently Asked Questions
What are the common symptoms of subclinical hypothyroidism and how can I recognize them?
Common symptoms include persistent fatigue that doesn't improve with rest, unexplained mild weight gain, increased sensitivity to cold, dry skin, hair thinning, mild depression or mood changes, difficulty concentrating, and constipation. These symptoms often develop gradually and may be subtle, making them easy to overlook or attribute to other factors like stress or aging.
What causes subclinical hypothyroidism and who is most at risk?
The most common cause is autoimmune thyroiditis, particularly Hashimoto's disease, where the immune system attacks thyroid tissue. Other causes include previous thyroid surgery, radiation treatment, or certain medications. Women over 60 face the highest risk, along with individuals having a family history of thyroid disease, autoimmune conditions, or previous thyroid problems.
When should subclinical hypothyroidism be treated with levothyroxine medication?
Treatment is typically recommended when TSH levels exceed 10 mIU/L or when TSH is between 4.5-10 mIU/L with symptoms, positive thyroid antibodies, pregnancy, cardiovascular risk factors, or other compelling clinical reasons. Treatment decisions should always be individualized based on symptoms, lab values, age, and overall health status in consultation with a healthcare provider.
How is subclinical hypothyroidism diagnosed through blood tests?
Diagnosis requires blood tests showing elevated TSH levels (usually above 4.5 mIU/L) while free T4 and T3 levels remain within normal ranges. Additional tests may include thyroid peroxidase antibodies to identify autoimmune causes. Healthcare providers often recommend repeat testing after 2-3 months to confirm persistent elevation before making treatment decisions.
Can subclinical hypothyroidism lead to serious health problems if left untreated?
Yes, untreated subclinical hypothyroidism may lead to cardiovascular complications, elevated cholesterol, cognitive decline, mood disorders, fertility problems in women, and pregnancy complications. There's also risk of progression to overt hypothyroidism, particularly in those with positive thyroid antibodies. However, not everyone develops complications, which is why treatment decisions are individualized.