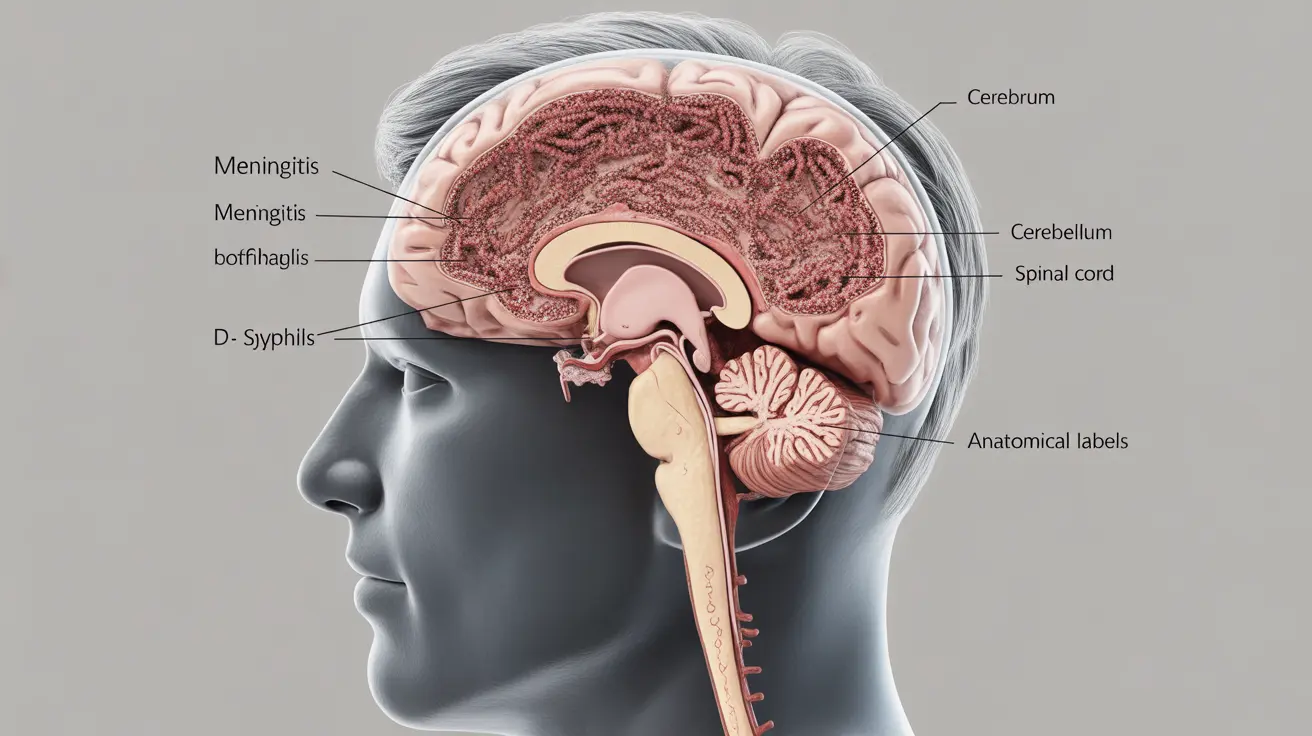
Syphilitic meningitis is a serious neurological complication that occurs when the bacteria causing syphilis spreads to the protective membranes surrounding the brain and spinal cord. This condition requires immediate medical attention, as early diagnosis and treatment are crucial for preventing long-term neurological damage.
While relatively rare in developed countries due to widespread antibiotic availability, understanding syphilitic meningitis remains important, particularly for healthcare providers and individuals at risk of syphilis infection. This article explores the key aspects of this condition, including symptoms, diagnosis, treatment options, and prevention strategies.
Early Signs and Symptoms
Recognizing the early signs of syphilitic meningitis is crucial for timely intervention. Common symptoms include:
- Severe headaches that persist
- Neck stiffness
- Sensitivity to light (photophobia)
- Nausea and vomiting
- Changes in mental status
- Vision problems
- Hearing difficulties
These symptoms typically develop within weeks to months after initial syphilis infection, though timing can vary significantly between individuals.
Diagnostic Process
Accurate diagnosis of syphilitic meningitis requires a comprehensive medical evaluation and specific testing procedures:
Laboratory Tests
- Cerebrospinal fluid (CSF) analysis
- Blood tests for syphilis (VDRL and RPR)
- Specific treponemal tests
Imaging Studies
Healthcare providers may order:
- MRI of the brain
- CT scan to rule out other conditions
- Specialized neurological assessments
Treatment Approaches
Treatment for syphilitic meningitis typically involves:
Primary Treatment
High-dose intravenous penicillin G is the standard treatment, usually administered for 10-14 days in a hospital setting. This approach ensures the medication can effectively cross the blood-brain barrier and target the infection.
Alternative Options
For patients allergic to penicillin, alternative antibiotics may be considered after careful desensitization procedures. Close monitoring during treatment is essential to ensure effectiveness and manage potential complications.
Prevention Strategies
Preventing syphilitic meningitis primarily involves preventing syphilis infection through:
- Safe sexual practices
- Regular STI screening
- Early treatment of primary syphilis
- Partner notification and testing
- Consistent use of barrier protection methods
Long-term Outlook and Complications
The prognosis for syphilitic meningitis varies depending on how quickly treatment begins. Early intervention typically leads to better outcomes, while delayed treatment can result in permanent neurological damage.
Frequently Asked Questions
What are the common symptoms of syphilitic meningitis and how can I recognize them early?
Common symptoms include severe headaches, neck stiffness, sensitivity to light, nausea, mental status changes, and vision or hearing problems. Early recognition involves being aware of these symptoms, especially if there's a history of syphilis exposure or infection.
How is syphilitic meningitis diagnosed and what tests are needed?
Diagnosis involves CSF analysis through lumbar puncture, blood tests for syphilis (VDRL and RPR), and specific treponemal tests. Imaging studies like MRI or CT scans may also be necessary to evaluate the extent of neurological involvement.
What treatments are effective for syphilitic meningitis and how soon should they be started?
High-dose intravenous penicillin G is the most effective treatment and should be started immediately upon diagnosis. Treatment typically lasts 10-14 days and requires hospitalization for proper administration and monitoring.
Can syphilitic meningitis be prevented, and what steps reduce the risk of developing it?
Prevention focuses on avoiding syphilis infection through safe sexual practices, regular STI screening, and prompt treatment of primary syphilis. Partner notification and testing are also crucial preventive measures.
What are the long-term complications if syphilitic meningitis is left untreated?
Untreated syphilitic meningitis can lead to permanent neurological damage, including cognitive decline, vision loss, hearing impairment, and other serious complications affecting the central nervous system. Some damage may be irreversible even after treatment.