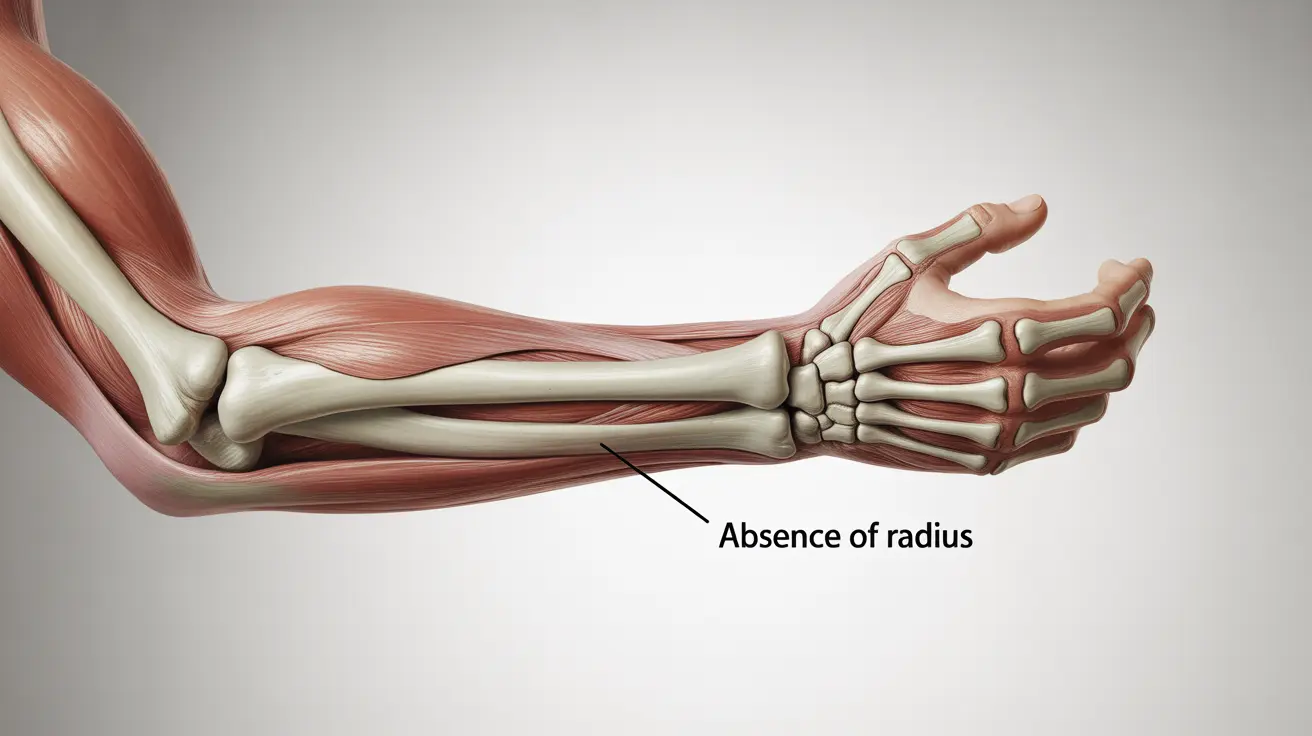
Thrombocytopenia-Absent Radius (TAR) Syndrome is a rare genetic condition characterized by two distinctive features: the absence of the radius bone in both arms and a consistently low blood platelet count. This complex condition affects both physical development and blood clotting abilities, requiring careful medical management from birth.
Understanding TAR Syndrome is crucial for affected families and healthcare providers to ensure proper care and support for individuals living with this condition. This comprehensive guide explores the key aspects of TAR Syndrome, including its symptoms, diagnosis, treatment options, and management strategies.
Key Features and Characteristics
TAR Syndrome presents with several distinctive characteristics that help medical professionals identify and diagnose the condition:
- Bilateral absence of the radius bones
- Consistently low platelet count (thrombocytopenia)
- Shortened forearms
- Presence of thumb (unlike some similar conditions)
- Hand and wrist positioning differences
Understanding the Genetic Component
TAR Syndrome has a complex genetic basis, typically involving mutations in the RBM8A gene. While the condition is inherited in an autosomal recessive pattern, its expression can vary significantly among affected individuals, making genetic counseling an important aspect of family planning.
Clinical Manifestations and Symptoms
Physical Features
The physical manifestations of TAR Syndrome primarily affect the upper limbs:
- Bilateral absence of radius bones
- Shortened forearms
- Curved ulna
- Normal thumb development
- Possible hand and wrist positioning abnormalities
Blood-Related Symptoms
The hematological aspects of TAR Syndrome can cause various complications:
- Increased bleeding tendency
- Easy bruising
- Nosebleeds
- Potential internal bleeding risks
- Variable platelet counts throughout life
Diagnosis and Assessment
Diagnosis of TAR Syndrome typically involves multiple approaches:
- Physical examination
- Blood platelet count monitoring
- Genetic testing
- Skeletal imaging
- Prenatal screening in some cases
Treatment and Management Strategies
Managing TAR Syndrome requires a comprehensive approach:
- Regular platelet monitoring
- Possible platelet transfusions
- Physical and occupational therapy
- Orthopedic interventions when necessary
- Careful dietary management, especially in infants
Frequently Asked Questions
What are the symptoms of Thrombocytopenia-Absent Radius Syndrome (TAR Syndrome) and how is it diagnosed?
TAR Syndrome is characterized by the absence of radius bones in both arms and low platelet counts. Diagnosis involves physical examination, blood tests, genetic testing, and imaging studies to confirm the absence of radius bones and assess platelet levels.
How is TAR Syndrome typically treated, and what are the available management options?
Treatment involves a multidisciplinary approach including platelet transfusions when necessary, physical therapy, occupational therapy, and possible surgical interventions. Regular medical monitoring and supportive care are essential components of management.
What are the potential complications of TAR Syndrome, especially in terms of bleeding risks?
Major complications include increased bleeding risk due to low platelet counts, which can lead to easy bruising, nosebleeds, and potential internal bleeding. Physical limitations due to upper limb differences may also impact daily activities.
Is TAR Syndrome inherited, and what is the risk to other family members?
TAR Syndrome is inherited in an autosomal recessive pattern, typically involving mutations in the RBM8A gene. Parents who carry the gene mutation have a 25% chance of having an affected child in each pregnancy.
How does the avoidance of cow's milk affect the management of TAR Syndrome in infants?
Some infants with TAR Syndrome may show sensitivity to cow's milk protein, which can affect platelet counts. In these cases, avoiding cow's milk and using appropriate alternatives under medical supervision may help maintain better platelet levels.