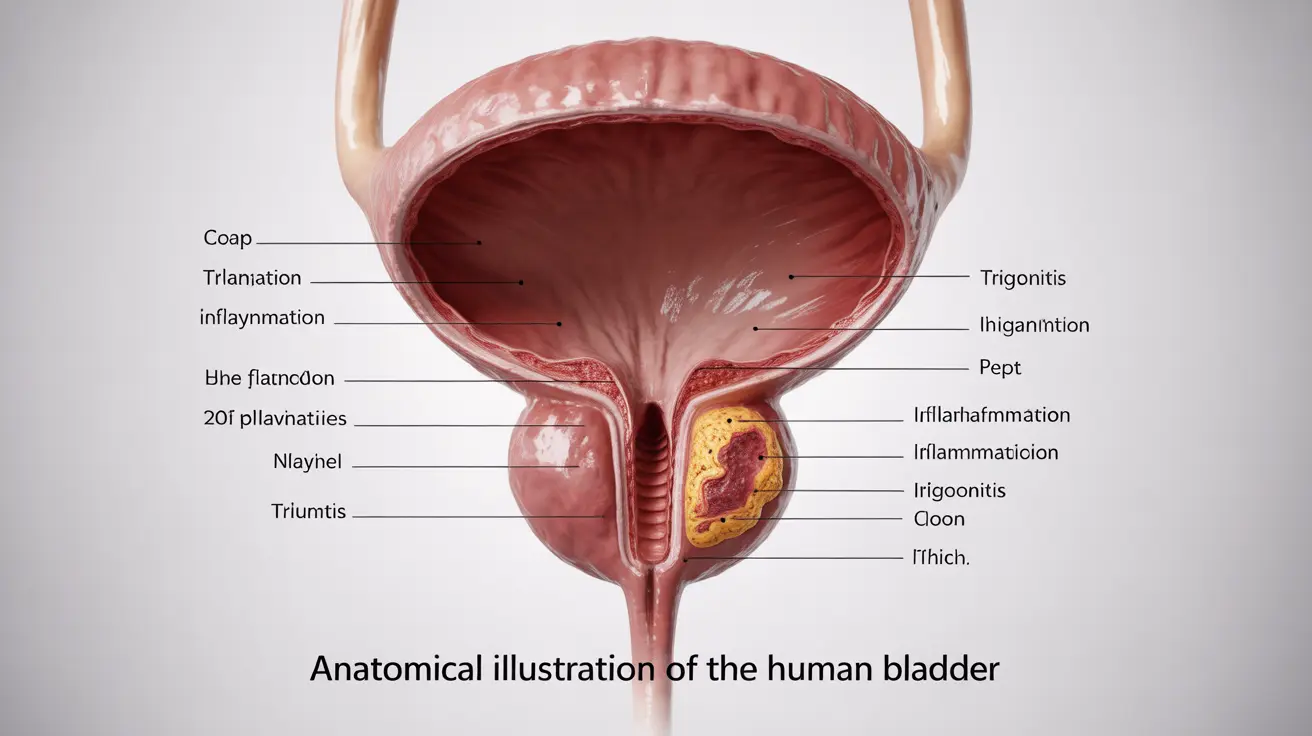
Trigonitis is a medical condition characterized by inflammation of the trigone, a triangular area located at the base of the bladder. This condition primarily affects women and can cause significant discomfort and urinary symptoms that may impact daily life. Understanding its symptoms, causes, and treatment options is crucial for proper management and relief.
While trigonitis shares some similarities with urinary tract infections (UTIs), it's a distinct condition that requires specific diagnosis and targeted treatment approaches. Let's explore this condition in detail to help you better understand its implications and management strategies.
Key Symptoms of Trigonitis
The symptoms of trigonitis can vary in intensity and may include:
- Frequent urination, especially during nighttime
- Urgent need to urinate
- Burning sensation during urination
- Lower abdominal pressure or discomfort
- Pelvic pain
- Bladder pain that worsens when the bladder is full
These symptoms can significantly impact quality of life and may be confused with other urinary conditions, making proper diagnosis essential.
Causes and Risk Factors
Several factors can contribute to the development of trigonitis:
Anatomical Factors
Women are more susceptible to trigonitis due to their shorter urethra and its proximity to potential sources of bacteria. The female anatomy makes it easier for bacteria to reach the bladder and trigger inflammation.
Hormonal Influences
Hormonal changes, particularly during menopause, can affect the urinary system's health. Decreased estrogen levels can lead to changes in the urinary tract tissue, potentially contributing to trigonitis development.
Other Contributing Factors
Additional risk factors include:
- Recurrent urinary tract infections
- Poor hygiene practices
- Certain medications
- Chronic health conditions
- Sexual activity
Diagnosis Process
Diagnosing trigonitis typically involves several steps:
- Physical examination
- Detailed medical history review
- Urinalysis to rule out infection
- Cystoscopy in some cases
- Imaging studies when necessary
Healthcare providers must differentiate trigonitis from other conditions with similar symptoms to ensure appropriate treatment.
Treatment Approaches
Treatment for trigonitis often involves a multi-faceted approach:
Medical Interventions
- Anti-inflammatory medications
- Antibiotics if bacterial infection is present
- Hormone therapy in some cases
- Bladder instillations
Lifestyle Modifications
Several lifestyle changes can help manage symptoms:
- Increasing water intake
- Avoiding bladder irritants
- Practicing good hygiene
- Regular pelvic floor exercises
- Stress management techniques
Prevention Strategies
While not all cases of trigonitis can be prevented, certain measures can reduce risk:
- Maintaining proper hydration
- Practicing good hygiene
- Urinating after sexual activity
- Wearing breathable cotton underwear
- Regular medical check-ups
Frequently Asked Questions
What are the common symptoms that indicate trigonitis in women?
Common symptoms include frequent urination, urgent need to urinate, burning sensation during urination, lower abdominal pressure, and bladder pain that intensifies when the bladder is full.
How is trigonitis diagnosed and how can it be distinguished from a urinary tract infection?
Trigonitis is diagnosed through physical examination, medical history review, urinalysis, and sometimes cystoscopy. Unlike UTIs, trigonitis may show negative bacterial cultures while still presenting urinary symptoms.
What causes trigonitis and which factors increase the risk of developing it?
Trigonitis can be caused by anatomical factors, hormonal changes, recurrent UTIs, and poor hygiene. Risk factors include being female, postmenopausal status, frequent UTIs, and certain medications.
What treatment options are available for managing trigonitis symptoms?
Treatment options include anti-inflammatory medications, antibiotics when necessary, hormone therapy, bladder instillations, and lifestyle modifications such as dietary changes and pelvic floor exercises.
Can hormonal changes or recurrent urinary tract infections lead to trigonitis?
Yes, both hormonal changes (especially during menopause) and recurrent urinary tract infections can contribute to the development of trigonitis by affecting the urinary tract tissue and creating conditions favorable for inflammation.