Hyperthyroidism occurs when your thyroid gland produces excessive amounts of thyroid hormones, but did you know there are several distinct types of this condition? Each type has unique causes, symptoms, and treatment approaches. Understanding these differences is crucial for proper diagnosis and management of the condition.
In this comprehensive guide, we'll explore the various types of hyperthyroidism, their specific characteristics, and how healthcare providers approach treatment for each form.
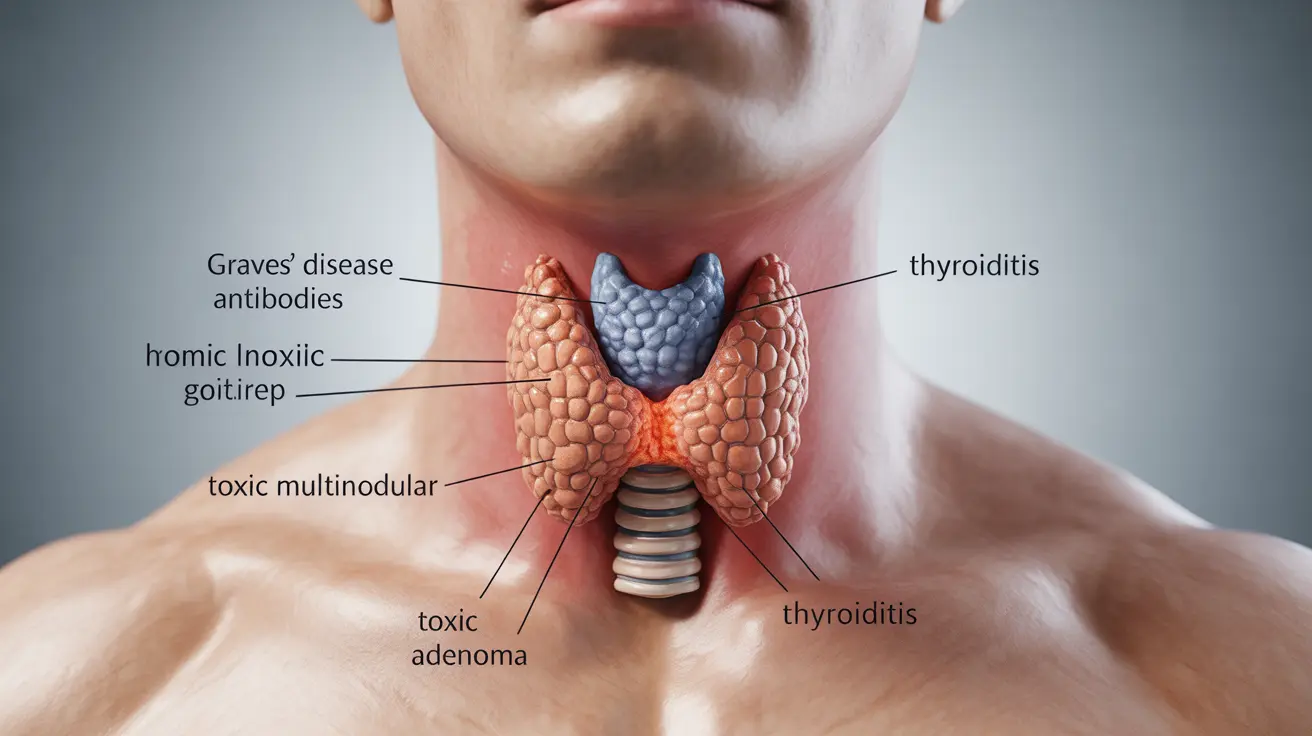
Common Types of Hyperthyroidism
Graves' Disease
Graves' disease is the most prevalent type of hyperthyroidism, accounting for up to 80% of cases. This autoimmune condition occurs when your immune system produces antibodies that stimulate the thyroid gland to produce excess hormones. It typically affects women between ages 30 and 50, though it can occur at any age.
Toxic Multinodular Goiter
This type develops gradually over years, usually in older adults. Multiple nodules in the thyroid become overactive, leading to excess hormone production. Unlike Graves' disease, it's not caused by an autoimmune response but rather by gradual growth and increased function of thyroid tissue.
Toxic Adenoma
A single nodule in the thyroid becomes overactive and produces excess hormones independently of normal regulatory mechanisms. This condition typically affects middle-aged and older adults and is less common than other types.
Inflammation-Related Hyperthyroidism
Thyroiditis
This temporary form of hyperthyroidism occurs when the thyroid gland becomes inflamed, releasing stored hormones into the bloodstream. Several types exist:
- Subacute thyroiditis (often following viral infections)
- Postpartum thyroiditis (occurring after pregnancy)
- Silent thyroiditis (painless inflammation)
Medication and Iodine-Induced Hyperthyroidism
Some medications and excessive iodine intake can trigger hyperthyroidism. This type is usually temporary and resolves when the triggering factor is removed. Common causes include:
- Iodine-containing medications
- Amiodarone (heart medication)
- Contrast dyes used in medical imaging
Diagnosis and Testing
Proper diagnosis of hyperthyroidism type requires several tests:
- Blood tests measuring thyroid hormone levels
- Radioactive iodine uptake tests
- Thyroid antibody tests
- Thyroid scans
- Physical examination
Treatment Approaches
Treatment varies significantly depending on the type of hyperthyroidism:
- Antithyroid medications
- Radioactive iodine therapy
- Surgery (thyroidectomy)
- Beta-blockers for symptom management
- Observation (for temporary forms)
Frequently Asked Questions
What are the different types of hyperthyroidism and how do their causes differ?
The main types include Graves' disease (autoimmune), toxic multinodular goiter (multiple overactive nodules), toxic adenoma (single overactive nodule), and thyroiditis (inflammation-related). Each has distinct causes: Graves' disease is autoimmune, while nodular conditions develop from abnormal tissue growth, and thyroiditis results from inflammation.
What symptoms should I look for to identify if I have Graves' disease versus other types of hyperthyroidism?
While all types share common symptoms like anxiety, weight loss, and rapid heartbeat, Graves' disease uniquely presents with eye problems (Graves' ophthalmopathy) and skin changes. Other types typically show more gradual symptom onset and lack these specific features.
How is hyperthyroidism diagnosed and what tests distinguish the various types?
Diagnosis involves blood tests measuring thyroid hormones (TSH, T3, T4), radioactive iodine uptake tests to determine how the thyroid processes iodine, and antibody tests specifically for Graves' disease. Thyroid scans can help identify nodules in toxic multinodular goiter and adenomas.
What are the common treatment options for toxic multinodular goiter compared to Graves' disease?
Toxic multinodular goiter often requires definitive treatment through radioactive iodine therapy or surgery. Graves' disease may be treated with antithyroid medications first, with radioactive iodine or surgery as secondary options if medication fails.
Can hyperthyroidism caused by thyroiditis or iodine intake resolve on its own, and how is it managed?
Yes, thyroiditis and iodine-induced hyperthyroidism often resolve spontaneously. Management typically involves symptom control with beta-blockers while waiting for the condition to improve. Avoiding excess iodine intake and monitoring thyroid function are key components of management.