Atrial fibrillation, commonly known as AFib, affects millions of Americans and represents one of the most prevalent heart rhythm disorders. This condition occurs when the heart's upper chambers (atria) beat irregularly and often rapidly, disrupting the normal blood flow throughout the body. Understanding the different types of AFib is crucial for patients and healthcare providers alike, as each classification requires distinct management approaches and carries varying levels of risk.
The classification system for atrial fibrillation helps medical professionals determine the most appropriate treatment strategy, assess stroke risk, and provide patients with accurate prognoses. By recognizing the characteristics of each type, individuals can work more effectively with their healthcare teams to manage their condition and maintain optimal heart health.
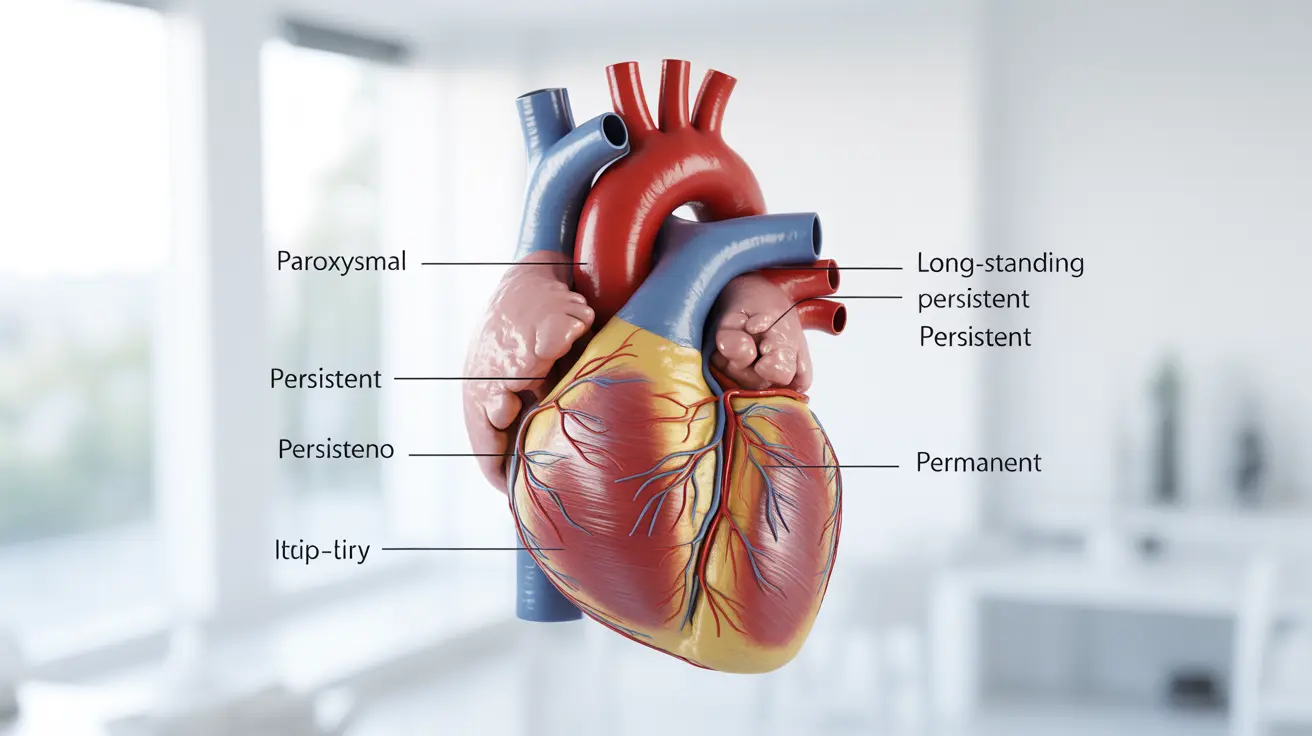
The Four Primary Classifications of Atrial Fibrillation
Medical experts categorize atrial fibrillation into four distinct types based primarily on the duration and pattern of episodes. This classification system, established by leading cardiology organizations, provides a framework for understanding how AFib progresses and responds to treatment.
Paroxysmal Atrial Fibrillation
Paroxysmal AFib represents the mildest form of the condition, characterized by episodes that begin suddenly and terminate spontaneously within seven days. Most paroxysmal episodes actually resolve within 24 hours without medical intervention. During these episodes, patients may experience symptoms such as palpitations, chest discomfort, shortness of breath, or fatigue, though some individuals remain completely asymptomatic.
The intermittent nature of paroxysmal AFib can make diagnosis challenging, as patients may visit their doctor when symptoms have already subsided. Heart rhythm monitoring devices, such as Holter monitors or event recorders, often prove essential for capturing these transient episodes and confirming the diagnosis.
Persistent Atrial Fibrillation
When AFib episodes last longer than seven days or require medical intervention to restore normal rhythm, the condition is classified as persistent. Unlike paroxysmal AFib, persistent episodes do not self-terminate and typically require cardioversion procedures, either through medication or electrical shock therapy, to return the heart to its normal rhythm.
Persistent AFib often indicates progression of the underlying condition and may signal that the heart's electrical system has undergone more significant changes. Patients with persistent AFib generally require more aggressive management strategies and closer monitoring to prevent complications.
Long-Standing Persistent Atrial Fibrillation
This classification applies when continuous AFib persists for twelve months or longer. Long-standing persistent AFib represents a more advanced stage of the condition, where the irregular rhythm has become deeply established in the heart's electrical system. At this stage, the atria may have undergone structural changes that make it increasingly difficult to maintain normal rhythm even after successful cardioversion.
Treatment approaches for long-standing persistent AFib often focus on rate control rather than rhythm control, as maintaining normal rhythm becomes progressively more challenging with extended duration of the condition.
Permanent Atrial Fibrillation
Permanent AFib is diagnosed when both the patient and physician have decided to accept the irregular rhythm as the ongoing heart rhythm. This decision typically occurs after multiple unsuccessful attempts at rhythm control or when the risks of continued rhythm control strategies outweigh the potential benefits. The term "permanent" reflects a treatment decision rather than an irreversible medical condition.
Patients with permanent AFib focus on managing heart rate and preventing complications, particularly stroke prevention through appropriate anticoagulation therapy. Quality of life and symptom management become primary treatment goals in this classification.
Treatment Approaches Based on AFib Type
The specific type of AFib significantly influences treatment decisions, with strategies ranging from watchful waiting to aggressive interventions. Treatment plans typically incorporate two main objectives: managing the irregular rhythm and preventing stroke-related complications.
Rhythm Control Strategies
For paroxysmal and some cases of persistent AFib, healthcare providers often pursue rhythm control strategies aimed at maintaining normal heart rhythm. These approaches may include antiarrhythmic medications, electrical cardioversion, or catheter ablation procedures. Younger patients with fewer underlying health conditions typically benefit most from rhythm control approaches.
Rate Control Management
Rate control strategies focus on slowing the heart rate during AFib episodes rather than eliminating the irregular rhythm entirely. This approach often proves more practical for patients with long-standing persistent or permanent AFib. Medications such as beta-blockers, calcium channel blockers, or digoxin help maintain heart rates within acceptable ranges while allowing patients to function normally.
Impact on Stroke Risk Assessment
All types of AFib increase stroke risk due to the potential for blood clot formation in the irregularly contracting atria. However, the classification of AFib influences how healthcare providers assess and manage this risk. The CHA2DS2-VASc scoring system helps determine appropriate anticoagulation therapy regardless of AFib type, but the frequency and duration of episodes may influence monitoring requirements and medication adherence strategies.
Patients with any type of AFib who have additional stroke risk factors typically require long-term anticoagulation therapy. The choice between different anticoagulant medications often depends on individual patient factors rather than the specific AFib classification.
Frequently Asked Questions
What are the four main types of atrial fibrillation and how do they differ?
The four main types of AFib are paroxysmal (self-terminating episodes lasting less than 7 days), persistent (episodes lasting more than 7 days requiring intervention), long-standing persistent (continuous AFib for 12 months or longer), and permanent (accepted as the ongoing rhythm). They differ primarily in duration, frequency, and whether episodes resolve spontaneously or require medical intervention to restore normal rhythm.
How is paroxysmal atrial fibrillation different from persistent and permanent AFib?
Paroxysmal AFib episodes start and stop on their own, typically within 24 hours and always within 7 days. Persistent AFib lasts longer than 7 days and requires medical treatment to restore normal rhythm. Permanent AFib is a treatment decision where the irregular rhythm is accepted as ongoing, usually after unsuccessful attempts at rhythm control or when rate control is deemed more appropriate.
What treatment options are available for each type of atrial fibrillation?
Paroxysmal AFib may be managed with "pill-in-the-pocket" antiarrhythmic drugs or catheter ablation. Persistent AFib often requires cardioversion, ongoing antiarrhythmic medications, or ablation procedures. Long-standing persistent AFib typically focuses on rate control medications and stroke prevention. Permanent AFib management emphasizes rate control drugs, anticoagulation for stroke prevention, and symptom management.
Can atrial fibrillation episodes stop on their own or do they always require medical intervention?
Paroxysmal AFib episodes stop on their own without medical intervention, typically within 24 hours. Persistent, long-standing persistent, and permanent AFib do not self-terminate and require medical management. However, even self-terminating episodes may benefit from preventive treatments to reduce frequency and duration of future episodes.
How does the classification of AFib affect the management and prevention of stroke risk?
While all AFib types carry stroke risk, classification influences monitoring frequency and treatment approaches. Paroxysmal AFib may require more frequent monitoring to ensure adequate anticoagulation coverage. Persistent and permanent AFib allow for more consistent anticoagulation strategies. The stroke prevention approach using CHA2DS2-VASc scoring remains consistent across all types, but medication adherence strategies and monitoring protocols may vary based on episode patterns.