Parkinson's disease affects millions of people worldwide, but many don't realize that this neurological condition isn't just one single disorder. There are actually several distinct types of Parkinson's disease, each with unique characteristics, causes, and progression patterns that can significantly impact treatment approaches and patient outcomes.
Understanding these different classifications is crucial for patients, families, and caregivers as it helps explain why symptoms and treatment responses can vary so dramatically between individuals. By exploring the various types of Parkinson's disease, we can better comprehend this complex condition and make more informed decisions about care and management strategies.
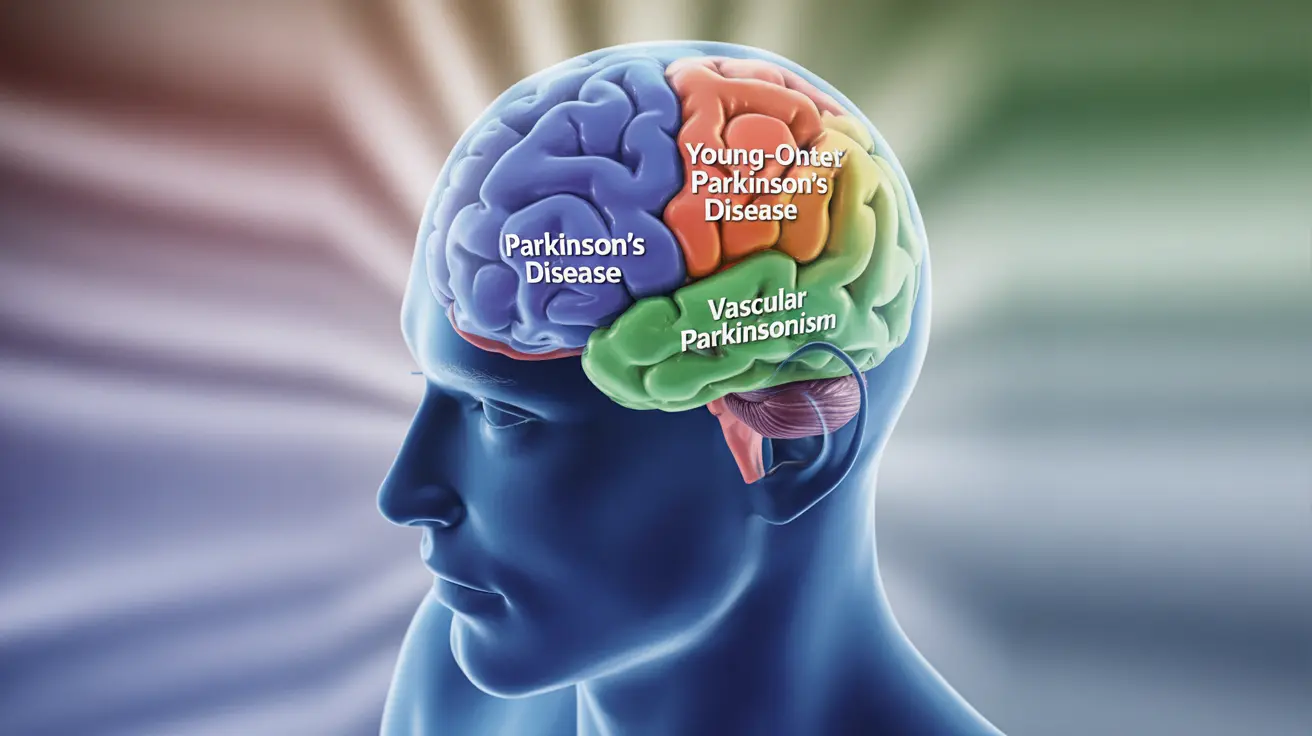
Primary Types of Parkinson's Disease
Idiopathic Parkinson's Disease
Idiopathic Parkinson's disease represents the most common form, accounting for approximately 85-90% of all cases. The term "idiopathic" means the exact cause remains unknown, though researchers have identified several contributing factors including genetic predisposition, environmental toxins, and age-related cellular changes.
This classical form typically develops gradually, with symptoms appearing subtly and progressing over years. Patients usually experience the characteristic motor symptoms: tremor at rest, muscle rigidity, bradykinesia (slowness of movement), and postural instability. Non-motor symptoms such as sleep disturbances, depression, and cognitive changes may also emerge as the condition advances.
Young-Onset Parkinson's Disease
When Parkinson's disease develops before age 50, it's classified as young-onset Parkinson's disease (YOPD). This form affects roughly 10-20% of all Parkinson's patients and often has a stronger genetic component compared to typical late-onset cases.
YOPD frequently presents with different symptom patterns, including more prominent dystonia (involuntary muscle contractions) and less cognitive decline in the early stages. Patients with young-onset disease may experience better responses to medication initially but are more likely to develop movement complications from long-term treatment.
Secondary Forms of Parkinsonism
Drug-Induced Parkinsonism
Drug-induced parkinsonism occurs when medications block dopamine receptors in the brain, mimicking Parkinson's disease symptoms. Common culprits include antipsychotic medications, certain anti-nausea drugs, and some blood pressure medications containing reserpine.
Unlike idiopathic Parkinson's disease, drug-induced parkinsonism typically affects both sides of the body equally from the onset and may not include the classic resting tremor. The condition often develops within weeks to months of starting the offending medication.
Vascular Parkinsonism
Vascular parkinsonism results from small strokes or reduced blood flow to specific brain regions that control movement. This form primarily affects the lower body, causing difficulty with walking and balance while often sparing the hands and arms initially.
Patients with vascular parkinsonism may experience a more stepwise progression rather than the gradual decline seen in idiopathic Parkinson's disease. Brain imaging typically reveals evidence of small vessel disease or multiple small strokes.
Genetic Variations and Hereditary Forms
Familial Parkinson's Disease
While most cases are sporadic, approximately 10-15% of Parkinson's disease cases have a clear genetic component. Several genes have been identified that can cause or increase the risk of developing Parkinson's disease, including LRRK2, PARKIN, PINK1, and SNCA.
Familial forms often have distinct characteristics depending on the specific genetic mutation involved. For example, LRRK2 mutations tend to cause symptoms very similar to idiopathic Parkinson's disease, while PARKIN mutations typically result in young-onset disease with slower progression.
Atypical Parkinsonism Disorders
Progressive Supranuclear Palsy (PSP)
PSP is a rare neurodegenerative disorder that shares some symptoms with Parkinson's disease but progresses more rapidly and affects additional brain areas. Key distinguishing features include difficulty with eye movements, particularly looking up and down, frequent falls, and speech difficulties.
Multiple System Atrophy (MSA)
MSA affects multiple body systems simultaneously, causing parkinsonism along with autonomic dysfunction (blood pressure changes, bladder problems) and cerebellar symptoms (coordination difficulties). This condition typically has a faster progression than idiopathic Parkinson's disease.
Dementia with Lewy Bodies (DLB)
DLB presents with cognitive symptoms alongside parkinsonism, with patients experiencing visual hallucinations, fluctuating alertness, and REM sleep behavior disorder. The cognitive symptoms in DLB typically appear earlier and more prominently than in Parkinson's disease dementia.
Diagnosis and Classification Methods
Accurate diagnosis of Parkinson's disease types requires comprehensive clinical evaluation by movement disorder specialists. The diagnostic process typically includes detailed medical history, physical examination, assessment of symptom patterns, and response to dopaminergic medications.
Advanced imaging techniques such as DaTscan (dopamine transporter imaging) can help distinguish between different forms of parkinsonism. Genetic testing may be considered for young-onset cases or those with strong family histories.
Progression Patterns and Prognosis
The rate of progression varies significantly among different types of Parkinson's disease. Idiopathic Parkinson's disease typically progresses gradually over 10-20 years, while atypical forms like PSP and MSA often advance more rapidly within 5-10 years.
Factors influencing progression include age at onset, genetic background, overall health status, and access to appropriate treatment. Young-onset patients often have slower disease progression but may face unique challenges related to career, family planning, and long-term medication effects.
Frequently Asked Questions
What are the different types of Parkinson's disease and how are they different from each other?
The main types include idiopathic Parkinson's disease (the most common form with unknown cause), young-onset Parkinson's disease (developing before age 50), drug-induced parkinsonism (caused by medications), vascular parkinsonism (from small strokes), and atypical forms like Progressive Supranuclear Palsy and Multiple System Atrophy. Each type has distinct symptoms, causes, and progression patterns that affect treatment approaches.
What causes drug-induced parkinsonism and can it go away if I stop taking the medication?
Drug-induced parkinsonism is caused by medications that block dopamine receptors in the brain, particularly antipsychotic drugs, certain anti-nausea medications, and some blood pressure treatments. In many cases, symptoms can improve or completely resolve within weeks to months after discontinuing the offending medication, though recovery may take longer in older patients or those who took medications for extended periods.
Is Parkinson's disease hereditary, and what does it mean if I have a family history of it?
While most Parkinson's disease cases are sporadic, about 10-15% have a genetic component. Having a family history increases your risk but doesn't guarantee you'll develop the condition. Specific gene mutations like LRRK2, PARKIN, and PINK1 can cause familial forms. If you have a strong family history, genetic counseling and testing may be beneficial to understand your personal risk and available options.
How do doctors diagnose which type of Parkinson's disease a person has?
Diagnosis involves comprehensive clinical evaluation including medical history, physical examination, symptom assessment, and medication response testing. Movement disorder specialists use specific diagnostic criteria, may perform DaTscan imaging to assess dopamine function, and consider genetic testing for young-onset or familial cases. The pattern of symptoms, progression rate, and treatment response help distinguish between different types.
Why do some types of Parkinson's progress faster than others, and what determines how quickly symptoms worsen?
Progression rates vary because different types affect different brain regions and systems. Atypical forms like Progressive Supranuclear Palsy typically progress faster than idiopathic Parkinson's disease because they damage multiple brain areas simultaneously. Factors influencing progression include age at onset, genetic background, overall health, brain reserve capacity, and access to appropriate treatment. Young-onset patients often have slower progression, while older patients may experience more rapid symptom development.