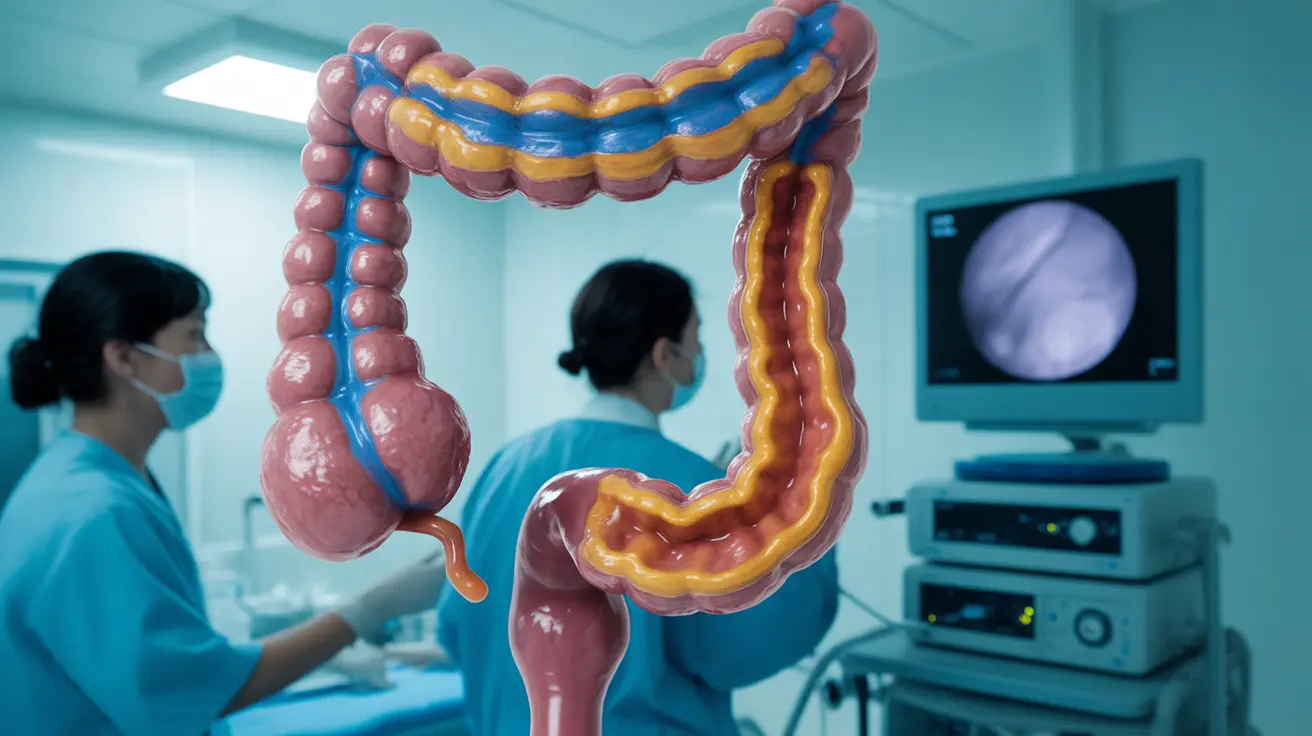
Living with ulcerative colitis (UC) means having specific medical needs, particularly when it comes to diagnostic procedures like colonoscopies. While colonoscopies are routine screening tools for the general population, they take on additional significance and require special considerations for individuals with ulcerative colitis.
Understanding these differences is crucial for both patients and healthcare providers to ensure effective disease monitoring and optimal outcomes. Let's explore how colonoscopies differ for UC patients and what special considerations need to be taken into account.
Key Differences in UC Colonoscopies
Colonoscopies for ulcerative colitis patients differ from regular screening colonoscopies in several important ways. The procedure requires more detailed examination of the colon lining, often takes longer to perform, and may need to be conducted more frequently to monitor disease activity and check for complications.
Enhanced Visualization Techniques
During a UC colonoscopy, doctors typically use specialized techniques such as chromoendoscopy, which involves applying dyes to the colon lining to highlight subtle changes in tissue. This enhanced visualization helps identify areas of inflammation, dysplasia, or early signs of cancer that might be harder to detect with standard colonoscopy methods.
Frequency of Colonoscopies for UC Patients
While individuals without inflammatory bowel disease typically begin routine colonoscopy screening at age 45, UC patients require more frequent examinations. The schedule depends on factors such as disease duration, extent of inflammation, and individual risk factors.
Monitoring Schedule Guidelines
Most UC patients should begin surveillance colonoscopies about 8-10 years after their initial diagnosis. The frequency may range from every 1-2 years, compared to every 10 years for routine screening in the general population. This increased frequency helps monitor disease activity and catch potential complications early.
Special Considerations for Sedation
UC patients often require different approaches to sedation during colonoscopy procedures. The inflammation and sensitivity associated with ulcerative colitis can make the procedure more uncomfortable, necessitating adjustments to standard sedation protocols.
Customized Sedation Approaches
Healthcare providers may opt for deeper sedation or different medication combinations to ensure patient comfort and procedure effectiveness. This is particularly important in cases where extensive examination is needed or when patients have experienced significant discomfort during previous procedures.
Cancer Surveillance in UC
Colonoscopy plays a crucial role in cancer prevention for UC patients, who have an increased risk of developing colorectal cancer. The procedure allows for detailed examination of the colon and the ability to take biopsies of suspicious areas.
Advanced Screening Methods
During UC colonoscopies, doctors typically take multiple biopsies throughout the colon, even from areas that appear normal. This systematic approach helps detect any precancerous changes that might not be visible to the naked eye.
Preparation Requirements
While the basic principle of bowel preparation remains similar, UC patients may need modified preparation protocols. The presence of inflammation can make the cleaning process more challenging and may require adjustments to standard preparation methods.
Specialized Preparation Guidelines
UC patients might need to start the preparation process earlier or use modified preparation solutions that are gentler on the inflamed intestinal tissue. Close coordination with healthcare providers is essential to determine the most appropriate preparation method.
Frequently Asked Questions
What is the difference between a colonoscopy for ulcerative colitis patients and a normal colonoscopy?
UC colonoscopies involve more detailed examination, specialized visualization techniques like chromoendoscopy, and multiple biopsies throughout the colon. The procedure typically takes longer and requires more careful inspection of the intestinal lining.How often should people with ulcerative colitis get a colonoscopy compared to someone without the condition?
UC patients typically need colonoscopies every 1-2 years starting 8-10 years after diagnosis, whereas people without UC generally need screening colonoscopies every 10 years starting at age 45.Why do patients with ulcerative colitis sometimes require higher sedation during colonoscopy?
The inflammation and sensitivity associated with UC can make the procedure more uncomfortable, often requiring deeper sedation or modified sedation protocols to ensure patient comfort and allow for thorough examination.How does colonoscopy help in detecting and preventing colon cancer in ulcerative colitis?
Colonoscopy enables early detection of precancerous changes through detailed examination and systematic biopsies throughout the colon, helping to prevent cancer development in UC patients who have an increased risk.What preparation is needed for a colonoscopy when you have ulcerative colitis, and is it different from regular colonoscopy prep?
UC patients may need modified preparation protocols, potentially starting earlier or using gentler solutions. The specific preparation method should be determined in consultation with healthcare providers to account for individual disease status and sensitivity.