For individuals living with severe ulcerative colitis that hasn't responded well to medication, ileostomy surgery can be a life-changing treatment option. This surgical procedure, while significant, often provides relief from debilitating symptoms and can dramatically improve quality of life for those struggling with advanced ulcerative colitis.
In this comprehensive guide, we'll explore when ileostomy surgery becomes necessary, what to expect from the procedure, and how it impacts daily life. Understanding these aspects can help you make informed decisions about your treatment journey.
When Is Ileostomy Surgery Recommended?
Doctors typically recommend ileostomy surgery for ulcerative colitis patients in several specific scenarios:
- Failure of medical therapy to control symptoms
- Severe complications such as toxic megacolon
- High risk of colorectal cancer
- Significant bleeding that can't be controlled
- Severe quality of life impairment
The decision to proceed with surgery is always made carefully, considering both the severity of the condition and the patient's overall health status.
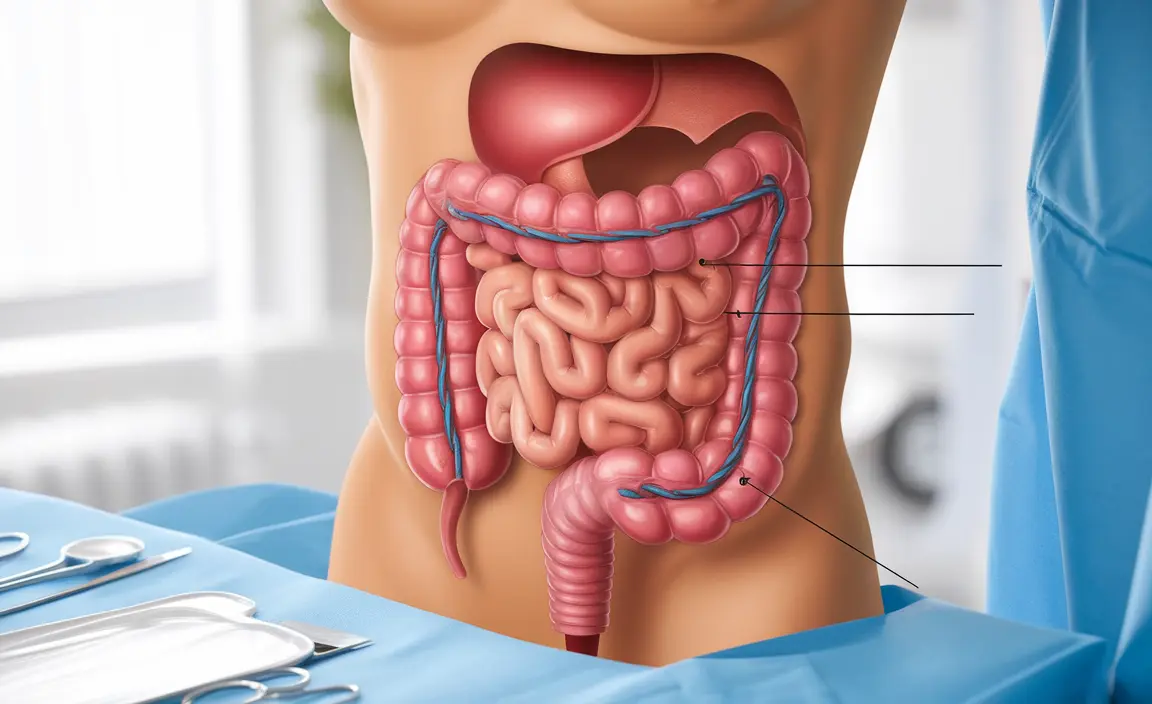
Understanding the Surgical Procedure
Total proctocolectomy with permanent ileostomy involves removing the entire colon and rectum, then creating a small opening (stoma) in the abdomen. The end of the small intestine (ileum) is brought through this opening, allowing waste to be collected in an external pouch.
Surgical Approaches
Modern surgical techniques include:
- Laparoscopic surgery (minimally invasive)
- Robotic-assisted procedures
- Traditional open surgery
- Single-incision laparoscopic surgery (SILS)
Recovery and Adaptation
Recovery from ileostomy surgery typically involves several stages:
- Initial hospital stay (4-7 days)
- Basic stoma care training
- Dietary modifications
- Gradual return to normal activities
- Regular follow-up appointments
Most patients can return to their regular activities within 4-6 weeks, though full recovery may take 2-3 months.
Living with an Ileostomy
Adapting to life with an ileostomy requires some lifestyle adjustments, but most people return to their normal activities, including:
- Work and social activities
- Exercise and sports
- Swimming and other water activities
- Intimate relationships
- Travel
Frequently Asked Questions
When is ileostomy surgery recommended for managing ulcerative colitis?
Ileostomy surgery is typically recommended when medical treatments fail to control symptoms, when there are severe complications like toxic megacolon, or when there's a high risk of colorectal cancer. It's also considered when the disease significantly impacts quality of life or causes uncontrollable bleeding.
What should I expect during and after a total proctocolectomy with permanent ileostomy?
During surgery, the entire colon and rectum are removed, and a stoma is created in the abdomen. After surgery, you'll spend 4-7 days in the hospital learning stoma care. Recovery continues at home for several weeks, during which you'll adapt to managing the ostomy system and gradually return to normal activities.
What are the common complications and risks associated with permanent ileostomy for ulcerative colitis?
Common complications can include skin irritation around the stoma, dehydration, blockage, infection, and potential stoma problems like prolapse or retraction. However, most complications are manageable with proper care and medical attention.
How does having a permanent ileostomy affect quality of life and sexual function?
While adjusting to an ileostomy requires adaptation, most people maintain a good quality of life. Sexual function can be preserved, though some patients may experience changes requiring adjustment. Support groups and specialized counseling can help address concerns and adaptation strategies.
Are there minimally invasive surgical options available for ulcerative colitis patients needing ileostomy?
Yes, minimally invasive options include laparoscopic and robotic-assisted surgery, which typically result in smaller incisions, less pain, and faster recovery compared to traditional open surgery. The specific approach depends on individual factors and surgeon expertise.