Living with ulcerative colitis (UC) often means paying close attention to changes in your stool, as these changes can signal disease activity and help guide treatment decisions. Understanding what's normal and what's not when it comes to ulcerative colitis stool patterns is crucial for managing the condition effectively.
This comprehensive guide will explore how ulcerative colitis affects bowel movements, what to watch for, and when changes in your stool warrant medical attention.
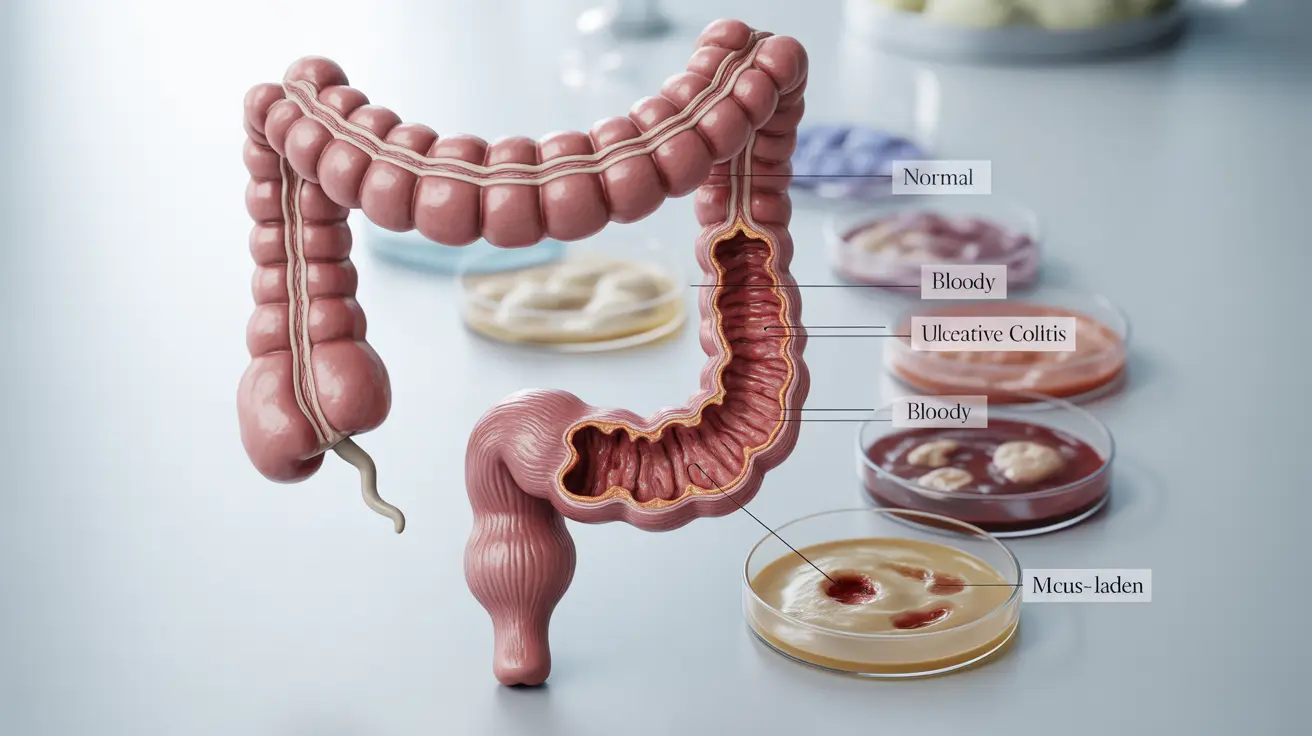
How Inflammation Affects Stool Appearance
Ulcerative colitis causes inflammation in the large intestine, which can significantly impact the appearance and consistency of your stool. During active inflammation, you may notice:
- Loose or watery stools
- Visible blood or pink-tinged stool
- Mucus in the stool
- Changes in stool color
- Irregular stool formation
Understanding Blood and Mucus in Stool
The presence of blood and mucus in stool is a hallmark sign of ulcerative colitis. When the intestinal lining becomes inflamed and develops ulcers, these can bleed and produce excess mucus. The blood may appear bright red, dark red, or make stools appear black, depending on where the bleeding occurs in the intestine.
The Diarrhea-Constipation Cycle
Many people with ulcerative colitis experience alternating periods of diarrhea and constipation. During flares, inflammation can speed up intestinal transit time, leading to diarrhea. However, when inflammation affects certain parts of the colon, it can also slow down transit time, resulting in constipation.
Managing Variable Bowel Movements
To help manage irregular bowel movements, consider:
- Keeping a symptom diary
- Following a consistent eating schedule
- Staying hydrated
- Working with your healthcare team to adjust medications as needed
- Identifying and avoiding trigger foods
Recognizing Flare-Up Symptoms
During an ulcerative colitis flare-up, stool-related symptoms often become more pronounced. Key indicators include:
- Increased frequency of bowel movements
- Urgent need to defecate
- Blood or mucus in stool
- Abdominal pain or cramping
- Changes in stool consistency
When to Seek Medical Care
Certain stool-related changes require immediate medical attention. Contact your healthcare provider if you experience:
- Large amounts of blood in your stool
- Severe abdominal pain
- High fever
- Extreme fatigue
- Signs of dehydration
- Inability to keep food or liquids down
Frequently Asked Questions
What does ulcerative colitis stool look like and how does inflammation affect its color and consistency?
Ulcerative colitis stool can vary in appearance, ranging from loose and watery to formed. During active inflammation, stools may contain visible blood, appear darker in color, or have a looser consistency. The presence of inflammation can also lead to mucus in the stool and irregular stool formation.
Why do people with ulcerative colitis experience blood and mucus in their stool?
Blood and mucus appear in stool because ulcerative colitis causes inflammation and ulcers in the intestinal lining. These ulcers can bleed, and the inflamed tissue produces excess mucus as a protective response. The amount of blood and mucus typically correlates with the severity of inflammation.
How can ulcerative colitis cause both diarrhea and constipation at different times?
The varying effects of inflammation on different parts of the colon can cause both diarrhea and constipation. Inflammation can speed up intestinal transit time, leading to diarrhea, or slow it down, causing constipation. The location and severity of inflammation determine which symptom predominates.
What are common stool-related symptoms during a flare-up of ulcerative colitis?
During a flare-up, common symptoms include increased bowel movement frequency, urgency to defecate, blood or mucus in stool, abdominal pain, and changes in stool consistency. These symptoms often occur alongside other systemic symptoms like fatigue and fever.
When should I seek urgent medical care for blood or changes in my stool if I have ulcerative colitis?
Seek immediate medical attention if you experience large amounts of blood in your stool, severe abdominal pain, high fever, extreme fatigue, signs of dehydration, or inability to keep food or liquids down. These symptoms may indicate a severe flare-up requiring prompt medical intervention.