For individuals living with ulcerative colitis (UC), understanding the relationship between this inflammatory bowel condition and colon cancer is crucial for maintaining long-term health. While these conditions share some similar symptoms, they are distinct diseases that require different approaches to diagnosis, monitoring, and treatment.
This comprehensive guide explores the important differences between ulcerative colitis and colon cancer, helping you understand the connection between these conditions and the steps needed for proper surveillance and early detection.
Key Differences in Symptoms and Presentation
While ulcerative colitis and colon cancer may share some overlapping symptoms, there are several distinctive characteristics that set them apart:
Ulcerative Colitis Symptoms
- Chronic diarrhea with blood or mucus
- Abdominal pain and cramping
- Urgency to have bowel movements
- Weight loss during flares
- Symptoms that come and go in cycles
- Fatigue and fever during flares
Colon Cancer Symptoms
- Persistent change in bowel habits
- Narrow, pencil-thin stools
- Unexplained weight loss
- Blood in stool that's dark or tar-like
- Constant fatigue
- Abdominal pain that doesn't improve
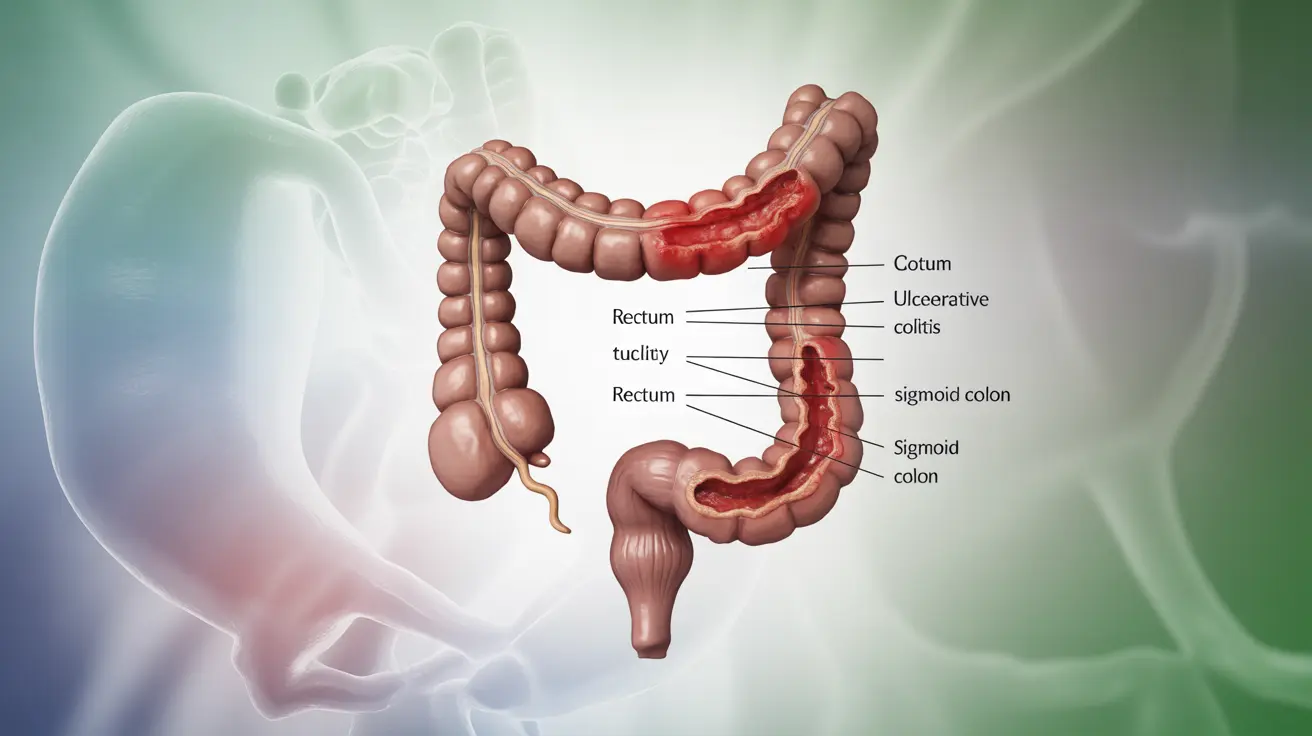
Understanding the UC-Cancer Connection
Having ulcerative colitis significantly increases the risk of developing colorectal cancer. This elevated risk is primarily due to chronic inflammation of the colon, which can lead to cellular changes over time.
The risk factors that contribute to cancer development in UC patients include:
- Duration of disease (particularly after 8-10 years)
- Extent of colon involvement
- Severity of inflammation
- Family history of colorectal cancer
- Presence of primary sclerosing cholangitis
Cancer Surveillance in UC Patients
Regular screening is essential for early detection of cancer or precancerous changes in UC patients. The surveillance protocol typically includes:
Timing of Screenings
- Initial screening 8 years after diagnosis for extensive colitis
- Earlier screening for patients with additional risk factors
- Regular follow-up colonoscopies every 1-2 years
- More frequent monitoring for high-risk patients
Screening Methods
- High-definition colonoscopy
- Chromoendoscopy
- Multiple biopsies throughout the colon
- Advanced imaging techniques when available
Managing Risk and Prevention
Several strategies can help reduce cancer risk in UC patients:
- Maintaining good disease control
- Taking prescribed medications consistently
- Regular medical follow-up
- Healthy lifestyle choices
- Smoking cessation
- Regular exercise and maintaining a healthy weight
Frequently Asked Questions
What are the main differences between ulcerative colitis and colon cancer symptoms?
The main differences lie in the pattern and persistence of symptoms. UC symptoms typically come and go in flares, while colon cancer symptoms tend to be more persistent and progressive. UC usually presents with bloody diarrhea and cramping, while colon cancer often shows as changes in bowel habits, unexplained weight loss, and dark or tar-like stools.
How does having ulcerative colitis increase my risk of developing colon cancer?
Chronic inflammation from UC can damage DNA in colon cells over time, potentially leading to cancerous changes. The risk increases with disease duration, extent of colon involvement, and severity of inflammation. Having UC can increase cancer risk by 2-3 times compared to the general population.
When should someone with ulcerative colitis start getting colonoscopy screenings for cancer surveillance?
Generally, cancer surveillance should begin 8 years after UC diagnosis for patients with extensive colitis. However, screening may start earlier for patients with additional risk factors such as family history or primary sclerosing cholangitis.
Can the inflammation in ulcerative colitis turn into colon cancer, and how is this monitored?
Yes, chronic inflammation can lead to cellular changes that may develop into cancer. This is monitored through regular colonoscopies with multiple biopsies, often using advanced imaging techniques to detect subtle changes in the colon lining.
What symptoms suggest colon cancer rather than a flare-up of ulcerative colitis?
Symptoms that suggest colon cancer include persistent changes in bowel habits, unexplained weight loss, dark or tar-like stools, constant fatigue, and abdominal pain that doesn't improve with usual UC treatments. Additionally, the presence of pencil-thin stools and symptoms that don't follow the typical pattern of UC flares should prompt immediate medical evaluation.