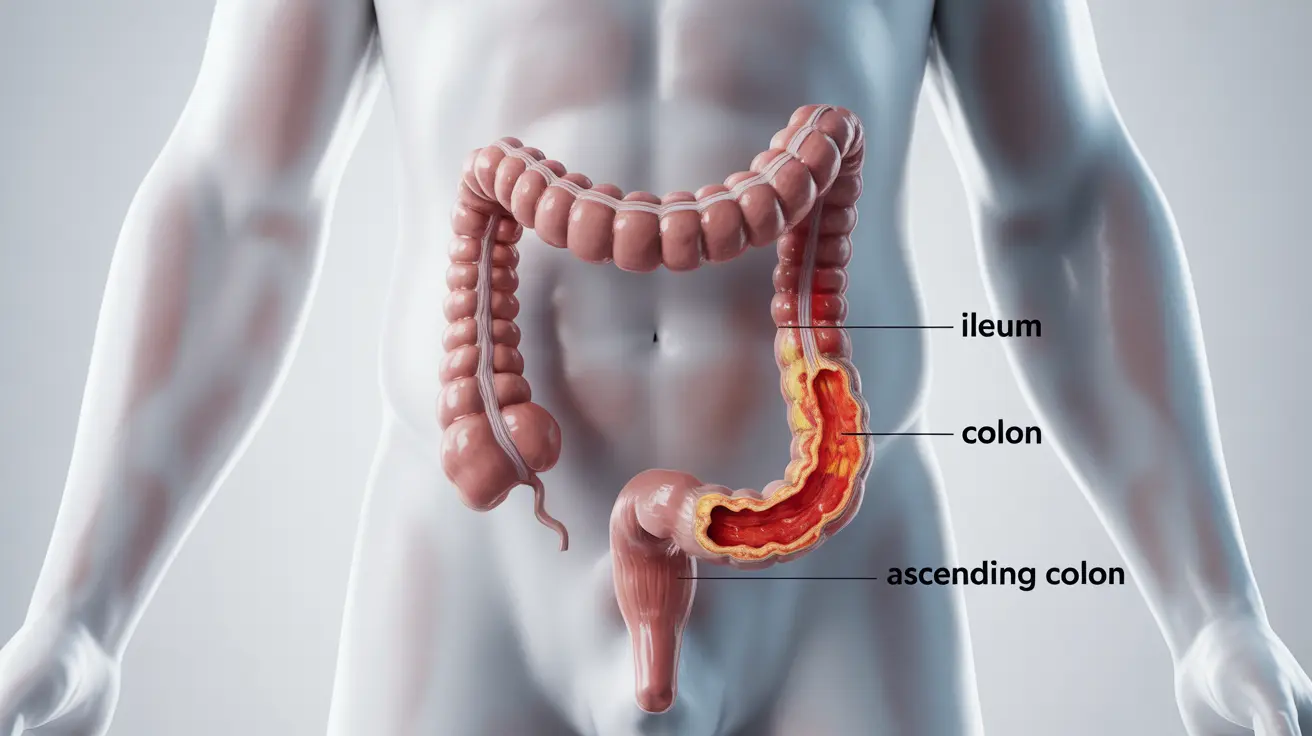
Ileocolitis is a form of inflammatory bowel disease (IBD) that specifically affects both the ileum (the last part of the small intestine) and the colon (large intestine). This condition most commonly occurs as part of Crohn's disease, causing inflammation and potential complications that can significantly impact a person's quality of life. Understanding its symptoms, diagnosis methods, and treatment options is crucial for managing the condition effectively.
What is Ileocolitis?
Ileocolitis represents a distinct pattern of intestinal inflammation where both the ileum and colon become inflamed, leading to various digestive symptoms and complications. This condition typically develops as part of Crohn's disease, though it can occasionally have other causes. The combination of inflammation in both areas can create unique challenges for diagnosis and treatment.
Common Signs and Symptoms
People with ileocolitis often experience a range of symptoms that can vary in severity and frequency. Understanding these symptoms is crucial for early detection and proper management:
- Abdominal pain, particularly in the lower right area
- Persistent diarrhea
- Unexplained weight loss
- Fatigue and weakness
- Loss of appetite
- Fever and night sweats
- Blood in stool
Diagnosis Process
Diagnosing ileocolitis requires a comprehensive medical evaluation and various diagnostic tests to confirm the condition and assess its severity. Healthcare providers typically use multiple approaches:
Physical Examination and Medical History
The diagnostic process begins with a thorough physical examination and detailed discussion of symptoms, medical history, and family history of inflammatory bowel diseases.
Diagnostic Testing
- Colonoscopy with biopsy
- CT enterography
- MR enterography
- Blood tests
- Stool samples
Treatment Approaches
Managing ileocolitis typically involves a multi-faceted treatment approach, tailored to each patient's specific symptoms and severity:
Medications
Various medications may be prescribed to control inflammation and manage symptoms:
- Anti-inflammatory drugs
- Immunosuppressants
- Biologics
- Antibiotics when necessary
- Pain relievers
Dietary Management
Diet plays a crucial role in managing ileocolitis symptoms. Key dietary considerations include:
- Identifying and avoiding trigger foods
- Maintaining proper nutrition
- Staying hydrated
- Following a low-residue diet during flares
- Working with a registered dietitian
Surgical Intervention
In some cases, surgery may be necessary to address complications or severe symptoms that don't respond to other treatments. Surgical options might include:
- Strictureplasty
- Bowel resection
- Removal of damaged tissue
Living with Ileocolitis
Successfully managing ileocolitis often requires lifestyle modifications and ongoing medical care. Regular check-ups, medication adherence, and stress management are essential components of long-term care. Many patients find success in combining conventional medical treatments with lifestyle changes and dietary modifications.
Frequently Asked Questions
- What are the common symptoms of ileocolitis and how can I recognize a flare-up?
Common symptoms include abdominal pain (especially in the lower right area), diarrhea, weight loss, and fatigue. A flare-up may be recognized by increased severity of these symptoms, along with fever, reduced appetite, and possible blood in stool.
- How is ileocolitis diagnosed by doctors, and what tests are involved?
Doctors diagnose ileocolitis through a combination of physical examination, medical history review, and diagnostic tests including colonoscopy, CT or MR enterography, blood tests, and stool samples. These tests help confirm the diagnosis and assess the extent of inflammation.
- What treatments are available for managing ileocolitis caused by Crohn's disease?
Treatment options include anti-inflammatory medications, immunosuppressants, biologics, and antibiotics. The treatment plan is typically personalized based on symptom severity and may include combinations of different medications.
- Can dietary changes help reduce symptoms or prevent flare-ups of ileocolitis?
Yes, dietary modifications can help manage symptoms. This includes identifying trigger foods, maintaining proper nutrition, staying hydrated, and possibly following a low-residue diet during flares. Working with a registered dietitian can help develop an appropriate meal plan.
- When is surgery necessary for ileocolitis, and what are the potential risks and benefits?
Surgery becomes necessary when medications fail to control symptoms, or complications such as strictures, fistulas, or severe bleeding develop. Benefits include symptom relief and improved quality of life, while risks include potential complications and the possibility of disease recurrence in other areas.