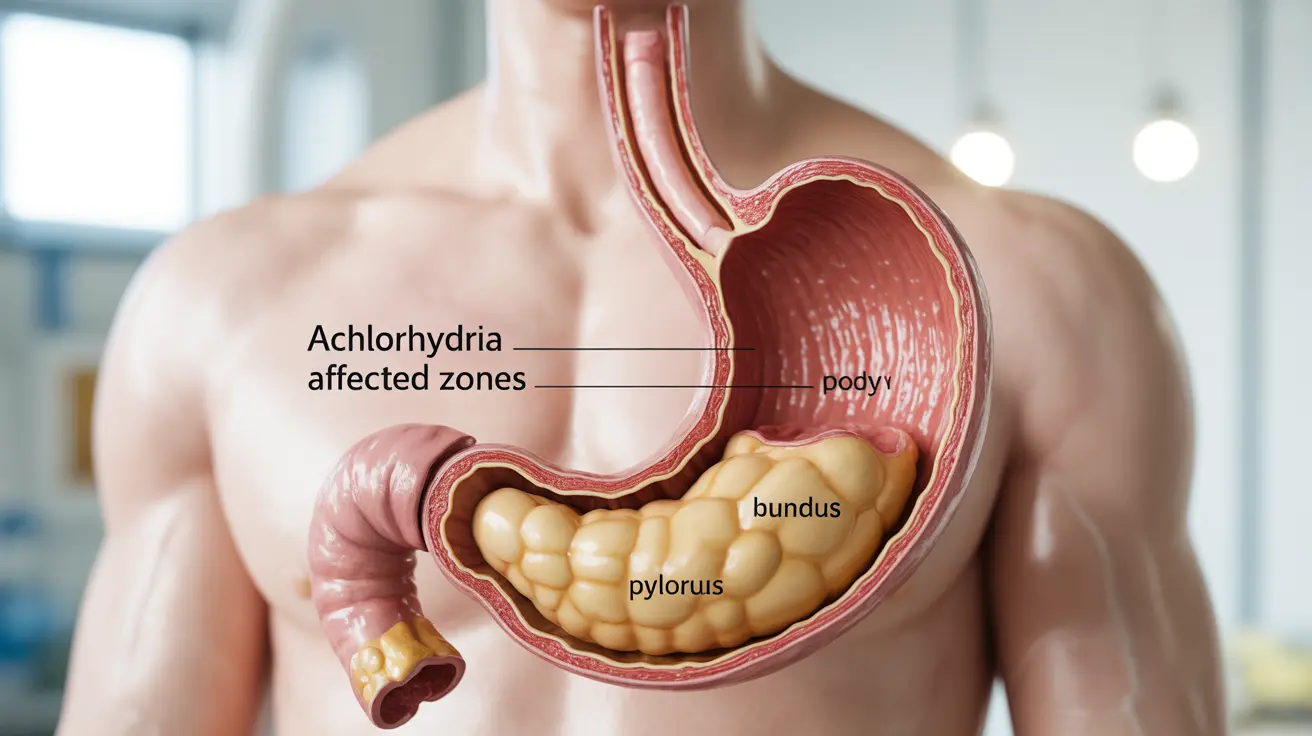
Achlorhydria is a serious digestive condition where the stomach fails to produce hydrochloric acid, a crucial component for proper digestion and nutrient absorption. This condition can significantly impact overall health and digestive function, leading to various complications if left untreated.
Understanding achlorhydria is essential for recognizing its symptoms early and seeking appropriate medical attention. This comprehensive guide explores the key aspects of achlorhydria, from its common signs to available treatment options.
Key Signs and Symptoms of Achlorhydria
Recognizing the symptoms of achlorhydria is crucial for early diagnosis and treatment. Common signs include:
- Bloating and gas after meals
- Feeling full quickly when eating
- Nausea and indigestion
- Upper abdominal discomfort
- Frequent burping
- Loss of appetite
More severe symptoms may develop over time, particularly related to nutrient deficiencies:
- Fatigue and weakness
- Brittle nails
- Hair loss
- Unexplained weight loss
- Anemia symptoms
- Neurological complications
Understanding the Causes and Risk Factors
Achlorhydria can develop due to various underlying conditions and factors:
Primary Causes
- Autoimmune gastritis
- Chronic H. pylori infection
- Stomach surgery
- Aging process
Risk Factors
Several factors can increase the likelihood of developing achlorhydria:
- Advanced age
- Family history of autoimmune conditions
- Long-term use of proton pump inhibitors
- Previous gastric surgery
- Chronic stress
Diagnostic Process
Healthcare providers use several methods to diagnose achlorhydria:
Testing Methods
- Gastric pH testing
- Endoscopy with biopsy
- Blood tests for nutrient deficiencies
- Gastrin level measurement
- H. pylori testing
Treatment Approaches
Treatment for achlorhydria typically involves a comprehensive approach:
Medical Interventions
- Addressing underlying conditions
- Supplemental acid replacement therapy
- Treatment of H. pylori infection if present
- Regular monitoring of nutrient levels
Dietary Management
Dietary modifications play a crucial role in managing achlorhydria:
- Eating smaller, more frequent meals
- Choosing easily digestible foods
- Avoiding trigger foods
- Taking prescribed supplements
Nutritional Considerations
People with achlorhydria often require specific nutritional support:
Essential Supplements
- Vitamin B12
- Iron
- Calcium
- Vitamin D
- Zinc
- Other minerals as needed
Frequently Asked Questions
What are the common symptoms and signs of achlorhydria to look out for?
Common symptoms include bloating, early satiety, indigestion, and upper abdominal discomfort. Long-term signs may include nutrient deficiencies leading to fatigue, brittle nails, and anemia.
What causes achlorhydria and which risk factors increase the likelihood of developing it?
Achlorhydria is primarily caused by autoimmune gastritis, H. pylori infection, and stomach surgery. Risk factors include advanced age, family history of autoimmune conditions, and long-term use of certain medications.
How is achlorhydria diagnosed and what tests are used to confirm it?
Diagnosis typically involves gastric pH testing, endoscopy with biopsy, blood tests for nutrient deficiencies, and gastrin level measurements. Healthcare providers may also test for H. pylori infection.
What treatment options are available for achlorhydria and how can underlying causes be managed?
Treatment options include addressing underlying conditions, acid replacement therapy, and treating H. pylori infections if present. Dietary modifications and regular medical monitoring are also essential components of management.
How does achlorhydria affect nutrient absorption and what dietary supplements might be needed?
Achlorhydria can significantly impair the absorption of vitamins and minerals, particularly B12, iron, and calcium. Patients often require supplementation of these nutrients along with vitamin D and zinc to prevent deficiencies.