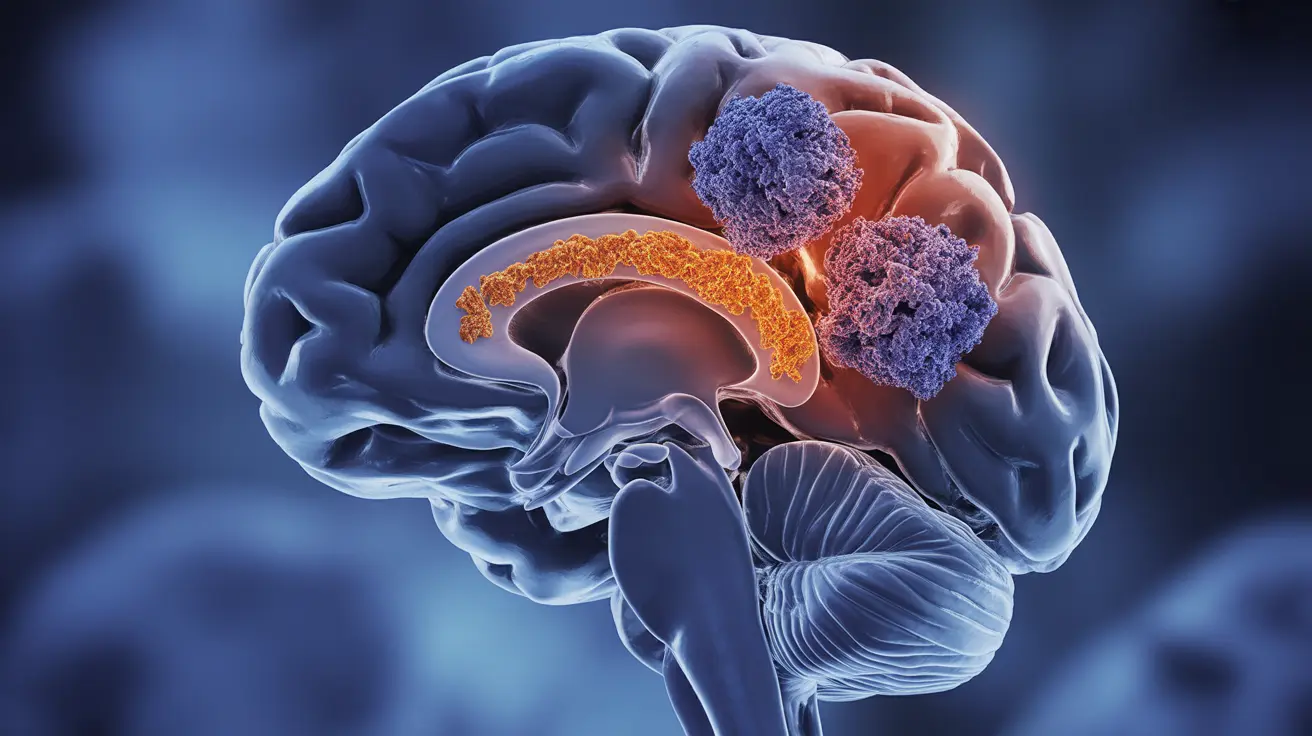
Autoimmune epilepsy is a complex neurological condition where the body's immune system mistakenly attacks healthy brain tissue, leading to seizures and other neurological symptoms. Unlike traditional forms of epilepsy, this condition requires a unique treatment approach focusing on both seizure management and immune system regulation.
Understanding this distinct type of epilepsy is crucial for healthcare providers and patients alike, as early recognition and appropriate treatment can significantly impact patient outcomes. This comprehensive guide explores the key aspects of autoimmune epilepsy, from its characteristic symptoms to the latest treatment approaches.
Key Characteristics and Symptoms
Autoimmune epilepsy often presents differently from traditional epilepsy forms. Patients typically experience:
- Frequent and severe seizures that develop suddenly
- Cognitive changes or memory problems
- Psychiatric symptoms such as anxiety or behavioral changes
- Resistance to conventional antiseizure medications
- Additional neurological symptoms like movement disorders
The seizures associated with autoimmune epilepsy can vary in type and severity, ranging from focal seizures affecting specific brain areas to more generalized seizures involving the entire brain.
Diagnostic Process and Testing
Diagnosing autoimmune epilepsy requires a comprehensive evaluation process that includes:
- Blood tests for specific antibodies
- Cerebrospinal fluid analysis
- MRI brain imaging
- Electroencephalogram (EEG) monitoring
- Comprehensive neurological examination
Healthcare providers often look for specific biomarkers and antibodies that indicate an autoimmune response targeting brain tissue. This diagnostic process is crucial for distinguishing autoimmune epilepsy from other forms of seizure disorders.
Treatment Approaches and Management
Immunotherapy Options
The primary treatment approach for autoimmune epilepsy focuses on immunotherapy, which may include:
- Corticosteroids for rapid inflammation reduction
- Intravenous immunoglobulin (IVIG) therapy
- Plasma exchange treatments
- Long-term immunosuppressive medications
Antiseizure Medication Role
While traditional antiseizure medications may be less effective in autoimmune epilepsy, they often play a supporting role in treatment. These medications may be used in combination with immunotherapy to help control seizure activity while the underlying immune response is addressed.
Long-term Management and Monitoring
Successfully managing autoimmune epilepsy requires ongoing monitoring and adjustment of treatment strategies. This includes:
- Regular neurological assessments
- Blood work to monitor immune system activity
- Tracking of seizure frequency and patterns
- Adjustment of medications as needed
- Management of potential side effects
Frequently Asked Questions
What are the common symptoms and seizure types seen in autoimmune epilepsy?
Autoimmune epilepsy typically presents with sudden-onset, frequent seizures that may be focal or generalized. Patients often experience additional symptoms including cognitive changes, memory problems, and psychiatric symptoms. The seizures are typically more resistant to standard antiseizure medications compared to traditional epilepsy.
How is autoimmune epilepsy diagnosed and what tests are involved?
Diagnosis involves multiple tests including blood work for specific antibodies, cerebrospinal fluid analysis, MRI brain imaging, and EEG monitoring. Doctors look for specific biomarkers that indicate autoimmune activity targeting the brain, along with clinical symptoms and response to treatment.
Why are standard antiseizure medications often ineffective for autoimmune epilepsy?
Standard antiseizure medications are less effective because they don't address the underlying immune system attack on brain tissue. These medications target seizure activity but don't suppress the autoimmune response that causes the seizures in the first place.
What immunotherapy treatments are available for managing autoimmune epilepsy?
Available immunotherapy treatments include corticosteroids, intravenous immunoglobulin (IVIG), plasma exchange, and long-term immunosuppressive medications. These treatments work by modulating the immune system response and reducing inflammation in the brain.
How important is early diagnosis and treatment for improving outcomes in autoimmune epilepsy?
Early diagnosis and treatment are crucial for improving outcomes in autoimmune epilepsy. Prompt intervention with appropriate immunotherapy can help prevent ongoing brain damage, reduce seizure frequency, and improve overall quality of life. Delays in treatment may lead to more severe symptoms and poorer long-term outcomes.