Cytopenia is a medical condition characterized by a reduction in one or more types of blood cells in the body. This condition can affect red blood cells, white blood cells, or platelets, and its impact on health can range from mild to severe depending on which cell types are affected and the extent of the deficiency.
Understanding cytopenia is crucial because blood cells play vital roles in our body, from carrying oxygen to fighting infections and preventing excessive bleeding. Early recognition and proper management of this condition can help prevent complications and improve outcomes for affected individuals.
Types of Cytopenia and Their Impact
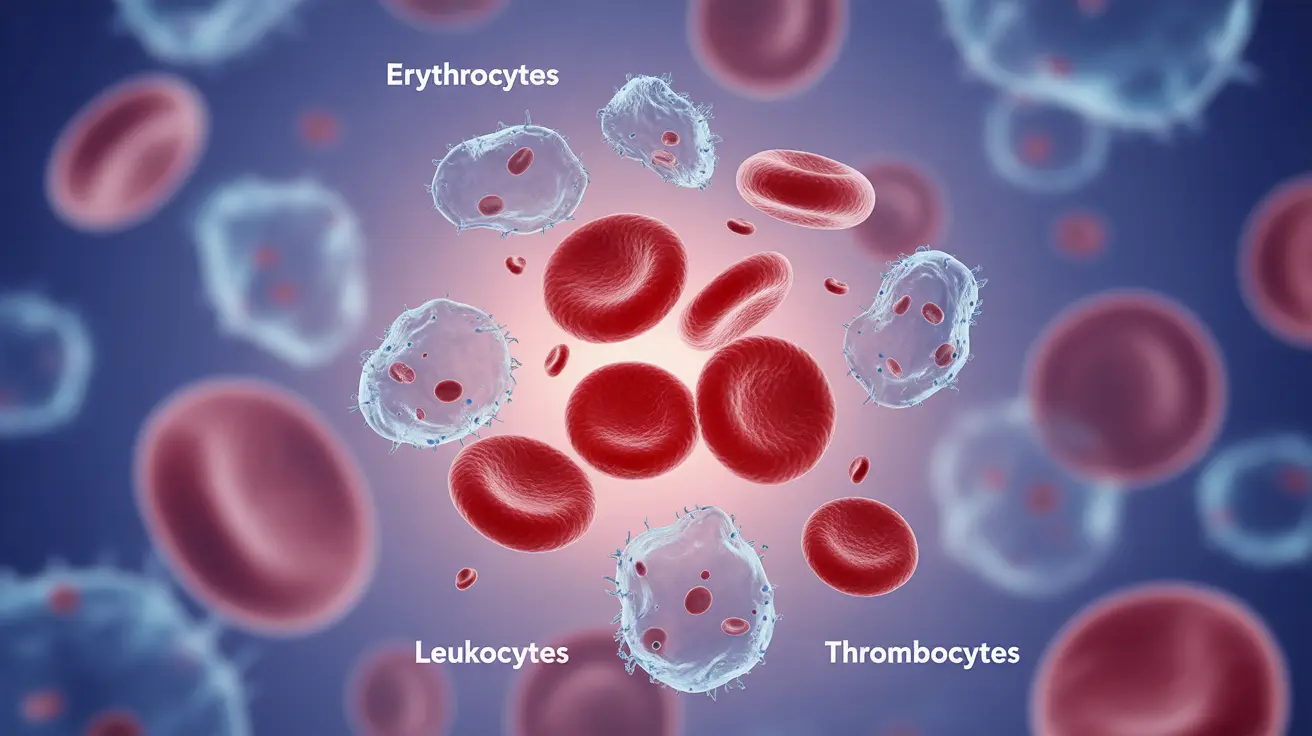
Cytopenia can manifest in several forms, depending on which blood cells are affected:
- Anemia (low red blood cells)
- Leukopenia (low white blood cells)
- Thrombocytopenia (low platelets)
- Pancytopenia (reduction in all three cell types)
Each type of cytopenia presents unique challenges and requires specific attention to manage effectively. The severity and impact on daily life can vary significantly among patients.
Signs and Symptoms of Cytopenia
The symptoms of cytopenia vary depending on which blood cells are affected. Common indicators include:
- Fatigue and weakness
- Frequent infections
- Easy bruising or bleeding
- Pale skin
- Shortness of breath
- Dizziness or lightheadedness
The presence and severity of these symptoms can help healthcare providers determine which type of cytopenia may be present and guide appropriate testing.
Diagnosis and Testing
Diagnosing cytopenia typically involves several steps:
- Complete blood count (CBC)
- Bone marrow examination
- Additional blood tests to identify underlying causes
- Medical history review
- Physical examination
These diagnostic tools help healthcare providers determine the type and severity of cytopenia, as well as identify any underlying conditions that may be contributing to the problem.
Treatment Approaches
Treatment for cytopenia depends on its underlying cause and severity. Common approaches include:
Medical Interventions
- Growth factor medications
- Blood transfusions
- Immunosuppressive therapy
- Treatment of underlying conditions
Nutritional Support
- Vitamin B12 supplementation
- Iron supplementation
- Folate supplementation
- Balanced diet rich in essential nutrients
Managing Cytopenia During Cancer Treatment
Cancer patients undergoing chemotherapy often experience cytopenia as a side effect. Management strategies include:
- Dose adjustments of chemotherapy
- Prophylactic antibiotics when necessary
- Regular blood count monitoring
- Growth factor support
- Transfusion support as needed
Frequently Asked Questions
What are the common symptoms that indicate I might have cytopenia?
Common symptoms include unusual fatigue, frequent infections, easy bruising or bleeding, pale skin, shortness of breath, and dizziness. The specific symptoms depend on which type of blood cells are affected.
What causes cytopenia and how is it diagnosed?
Cytopenia can be caused by various factors including bone marrow disorders, autoimmune conditions, medications, infections, and cancer treatments. Diagnosis typically involves blood tests, particularly a complete blood count (CBC), and may include bone marrow examination.
How is cytopenia treated and what are the available treatment options?
Treatment options include growth factor medications, blood transfusions, immunosuppressive therapy, and treating underlying conditions. The specific treatment plan depends on the cause and severity of the cytopenia.
Can nutritional deficiencies like vitamin B12 or folate deficiency lead to cytopenia?
Yes, nutritional deficiencies, particularly of vitamin B12, folate, and iron, can cause cytopenia. Addressing these deficiencies through supplementation and dietary changes often helps improve blood cell counts.
How can cytopenia be managed in patients undergoing cancer or chemotherapy treatments?
Management strategies include careful monitoring of blood counts, dose adjustments of chemotherapy when necessary, growth factor support, preventive antibiotics when appropriate, and blood transfusions as needed. Close coordination between oncology and hematology teams is essential.