Diabetic belly, a common concern among individuals with type 2 diabetes, refers to both the accumulation of visceral fat around the abdomen and potential digestive complications associated with the condition. Understanding this complex health issue is crucial for effective diabetes management and overall well-being.
This comprehensive guide explores the relationship between diabetes and abdominal changes, including the role of insulin resistance, gastroparesis, and practical strategies for managing these challenges.
The Connection Between Diabetes and Abdominal Changes
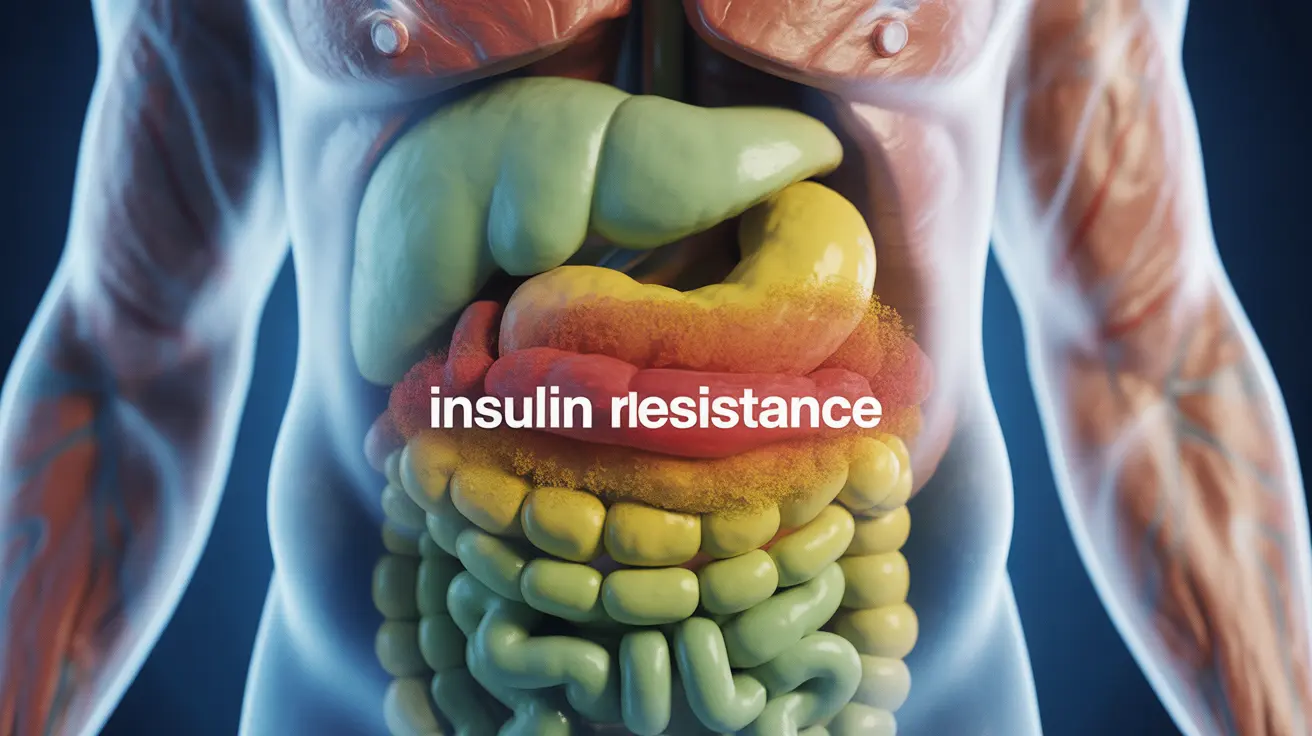
Type 2 diabetes significantly impacts how the body processes and stores fat, particularly in the abdominal area. When insulin resistance develops, the body struggles to properly regulate blood sugar levels, often leading to increased fat storage around vital organs. This type of fat, known as visceral fat, is particularly concerning due to its active role in metabolic dysfunction.
Understanding Visceral Fat and Its Impact
Visceral fat differs from subcutaneous fat (the kind you can pinch) because it surrounds internal organs and produces hormones that can increase inflammation and insulin resistance. This creates a challenging cycle where diabetes affects fat storage, and increased visceral fat makes diabetes management more difficult.
Health Risks Associated with Visceral Fat
The presence of excess visceral fat can lead to several complications:
- Increased insulin resistance
- Higher risk of cardiovascular disease
- Elevated blood pressure
- Greater inflammation throughout the body
- Reduced effectiveness of diabetes medications
Diabetic Gastroparesis and Abdominal Distention
Another significant factor contributing to diabetic belly is gastroparesis, a condition where high blood sugar levels damage the vagus nerve, leading to delayed stomach emptying. This condition can cause visible abdominal distention and various digestive symptoms.
Common Signs of Diabetic Gastroparesis
Key indicators include:
- Feeling full quickly during meals
- Bloating and visible abdominal distention
- Nausea and vomiting
- Unpredictable blood sugar levels
- Acid reflux and heartburn
Managing Diabetic Belly Through Lifestyle Changes
Effective management of diabetic belly requires a comprehensive approach focusing on both blood sugar control and healthy lifestyle habits:
Dietary Modifications
Key dietary strategies include:
- Eating smaller, more frequent meals
- Choosing foods with a low glycemic index
- Increasing fiber intake gradually
- Limiting processed foods and added sugars
- Staying well-hydrated throughout the day
Exercise and Physical Activity
Regular physical activity is crucial for managing both diabetes and abdominal fat:
- Combining aerobic exercise with strength training
- Engaging in moderate activity for at least 150 minutes weekly
- Including core-strengthening exercises
- Taking regular walking breaks throughout the day
Frequently Asked Questions
- What causes a diabetic belly and how is it linked to type 2 diabetes?
Diabetic belly is primarily caused by insulin resistance, which leads to increased visceral fat storage around the abdomen. When the body becomes resistant to insulin, it struggles to process glucose effectively, often resulting in fat accumulation around internal organs.
- What are the common symptoms of gastroparesis in people with diabetes and how does it affect the belly?
Common symptoms include bloating, early satiety, nausea, vomiting, and visible abdominal distention. Gastroparesis affects the belly by slowing down digestion, leading to food remaining in the stomach longer than normal, causing discomfort and irregular blood sugar levels.
- How can visceral fat lead to complications in diabetes and increase the size of the abdomen?
Visceral fat acts as an active endocrine organ, releasing inflammatory compounds and hormones that increase insulin resistance and inflammation. This creates a cycle that can worsen diabetes control and lead to further abdominal fat accumulation.
- What dietary and lifestyle changes can help reduce diabetic belly and improve metabolic health?
Effective changes include adopting a balanced diet rich in fiber and lean proteins, maintaining regular physical activity, managing stress levels, getting adequate sleep, and monitoring blood sugar levels consistently.
- How is diabetic gastroparesis treated and what are the options to manage its symptoms effectively?
Treatment options include dietary modifications (eating smaller, more frequent meals), medications to improve stomach emptying, blood sugar control, and in severe cases, medical procedures. Working with healthcare providers to develop a comprehensive management plan is essential.