Emphysema is a serious respiratory condition that progressively affects breathing and quality of life. Recognizing and understanding emphysema symptoms is crucial for early detection and proper management of this chronic lung disease. This comprehensive guide will help you identify key warning signs and understand when to seek medical attention.
Early Warning Signs and Initial Symptoms
The earliest signs of emphysema often develop gradually, making them easy to overlook or dismiss. Understanding these initial symptoms is crucial for early intervention:
- Shortness of breath, especially during physical activity
- Persistent, mild cough
- Feeling the need to clear your throat frequently
- Mild fatigue during everyday activities
Progressive Symptoms and Development
As emphysema advances, symptoms typically become more noticeable and begin to affect daily activities more significantly:
- Chronic cough with or without mucus
- Increased breathlessness, even during rest
- Wheezing or whistling sound while breathing
- Chest tightness
- Frequent respiratory infections
Advanced Stage Indicators
In later stages, emphysema symptoms can become severe and significantly impact quality of life:
- Difficulty breathing even when sitting still
- Blue or gray tinge to lips or fingernails
- Barrel chest appearance
- Significant weight loss
- Morning headaches due to reduced oxygen levels
Distinguishing Emphysema from Other Conditions
Several respiratory conditions can mimic emphysema symptoms. Key distinguishing factors include:
- Pattern of breathlessness (gradual onset versus sudden)
- Response to rest and activity
- Presence of specific triggers
- Associated symptoms
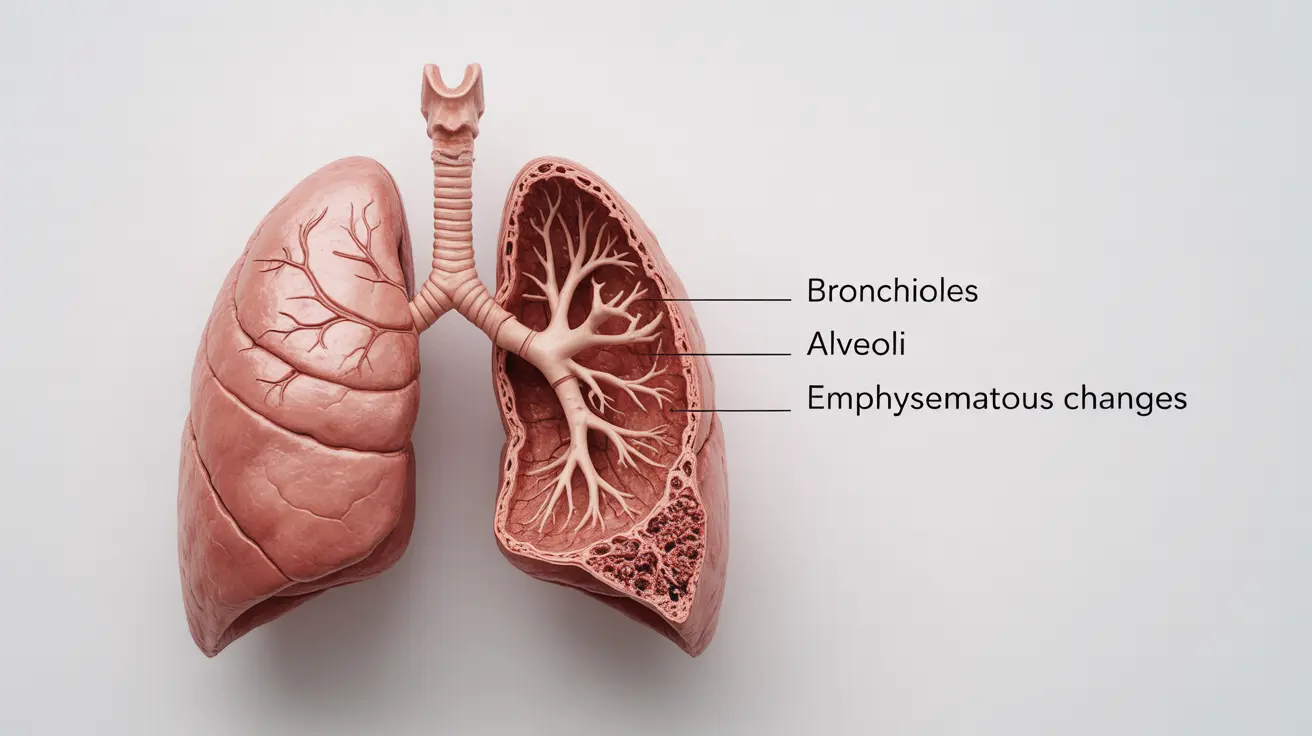
Diagnostic Process and Medical Assessment
Healthcare providers use various methods to confirm emphysema diagnosis:
- Physical examination and medical history review
- Pulmonary function tests
- Chest X-rays and CT scans
- Blood gas analysis
- Exercise tolerance tests
Managing Emphysema Through Lifestyle Changes
Several lifestyle modifications can help control symptoms and slow disease progression:
- Smoking cessation (the most crucial step)
- Regular moderate exercise within limitations
- Proper nutrition and hydration
- Stress management techniques
- Environmental modifications to reduce exposure to irritants
When to Seek Immediate Medical Attention
Certain symptoms require urgent medical care:
- Severe shortness of breath that comes on suddenly
- Inability to catch your breath even at rest
- Chest pain or rapid heartbeat
- Confusion or mental changes
- Fever with increased breathing difficulties
Frequently Asked Questions
What are the most common emphysema symptoms and how do they progress over time?
The most common symptoms begin with mild shortness of breath during activity and progress to chronic cough, persistent breathlessness, wheezing, and eventually difficulty breathing even at rest. The progression typically occurs over several years.
How can I tell if shortness of breath is caused by emphysema or something else?
Emphysema-related breathlessness typically develops gradually over time, worsens with activity, and improves little with rest. Unlike asthma or heart-related breathing problems, it's usually persistent and progressive rather than occurring in sudden episodes.
When should I seek medical help for worsening emphysema symptoms?
Seek immediate medical attention if you experience sudden worsening of breathlessness, inability to speak in full sentences, blue lips or fingernails, chest pain, or confusion. Regular follow-up is also important for monitoring gradual changes in symptoms.
What lifestyle changes can help manage or slow the progression of emphysema symptoms?
Key lifestyle changes include quitting smoking, avoiding secondhand smoke and air pollutants, participating in pulmonary rehabilitation, maintaining regular physical activity within your limits, and following a healthy diet.
How is emphysema diagnosed based on symptoms and medical tests?
Diagnosis typically involves a combination of physical examination, detailed medical history, pulmonary function tests, imaging studies (chest X-rays and CT scans), and sometimes blood gas analysis to assess oxygen levels.