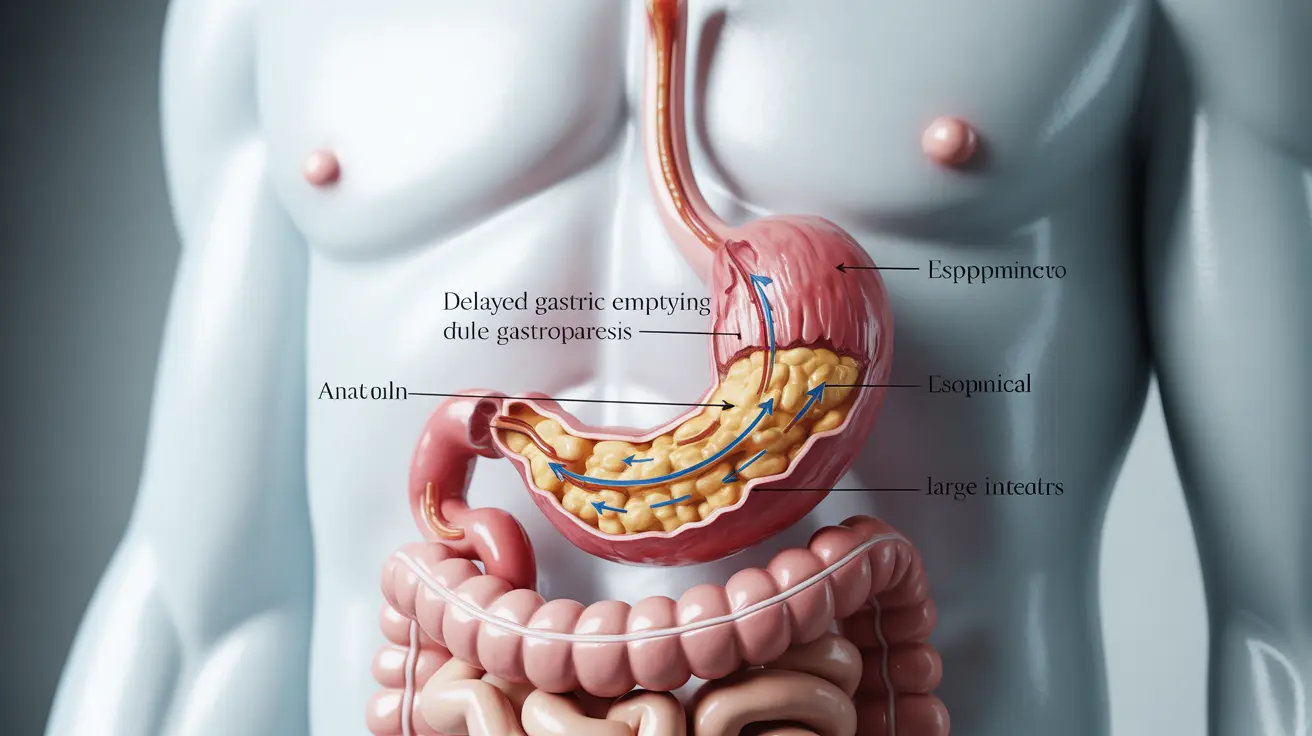
Gastroparesis is a complex digestive disorder that affects the normal movement of the stomach muscles, leading to delayed emptying of food into the small intestine. This condition can significantly impact quality of life and requires careful management through various treatment approaches and lifestyle modifications.
For individuals living with gastroparesis, understanding the condition's symptoms, causes, and available treatments is crucial for effective management and improved outcomes. This comprehensive guide explores everything you need to know about gastroparesis and how to manage its challenges.
What is Gastroparesis?
Gastroparesis occurs when the stomach muscles don't function properly, causing food to move too slowly through the digestive system. This delayed gastric emptying can lead to numerous complications and digestive issues that affect daily life and overall health.
Common Symptoms and Warning Signs
The symptoms of gastroparesis can vary in severity and may include:
- Feeling full quickly when eating
- Nausea and vomiting
- Bloating and abdominal pain
- Acid reflux or heartburn
- Unexplained weight loss
- Loss of appetite
These symptoms may fluctuate in intensity and can be particularly challenging to manage without proper medical guidance and lifestyle modifications.
Understanding the Causes
Several factors can contribute to the development of gastroparesis:
Diabetes-Related Gastroparesis
Diabetes is one of the most common causes of gastroparesis, as prolonged high blood sugar levels can damage the vagus nerve, which controls stomach muscle movement. Maintaining proper blood sugar control is essential for managing diabetes-related gastroparesis.
Other Common Causes
- Surgical complications
- Certain medications
- Neurological conditions
- Viral infections
- Autoimmune disorders
Dietary Management Strategies
Diet plays a crucial role in managing gastroparesis symptoms. Consider these dietary modifications:
- Eat smaller, more frequent meals
- Choose low-fiber, easily digestible foods
- Avoid high-fat meals
- Stay well-hydrated
- Consume liquid nutrients when solid foods are difficult to tolerate
Medical Treatment Options
Treatment for gastroparesis typically involves a combination of approaches:
Medications
Various medications can help manage symptoms and improve gastric emptying:
- Antiemetics for nausea
- Prokinetics to improve stomach emptying
- Pain management medications
- Acid-reducing medications
Advanced Treatment Options
For severe cases, additional treatments may include:
- Gastric electrical stimulation
- Feeding tubes in severe cases
- Surgical interventions when conservative treatments fail
When to Seek Emergency Care
Some symptoms require immediate medical attention:
- Severe abdominal pain
- Prolonged vomiting
- Signs of dehydration
- Inability to keep any food or liquids down
- High fever
- Blood in vomit
Frequently Asked Questions
What are the common symptoms of gastroparesis and how can I recognize them? Gastroparesis symptoms typically include early satiety, nausea, vomiting, bloating, and abdominal pain. These symptoms often occur regularly and can persist for extended periods, particularly after eating.
What dietary changes can help manage gastroparesis symptoms effectively? Focus on eating smaller, more frequent meals, choosing low-fiber foods, avoiding high-fat items, and staying well-hydrated. Consider a gastroparesis-friendly diet that emphasizes easily digestible foods and proper portion control.
How is gastroparesis treated, including medication and other medical options? Treatment typically involves medications like antiemetics and prokinetics, dietary modifications, and in severe cases, surgical interventions or gastric electrical stimulation. The approach is often personalized based on symptom severity and underlying causes.
Can diabetes cause gastroparesis, and how does blood sugar control affect the condition? Yes, diabetes is a leading cause of gastroparesis due to nerve damage from prolonged high blood sugar levels. Maintaining good blood sugar control is crucial for preventing and managing diabetic gastroparesis.
When should someone with gastroparesis seek emergency medical attention for complications? Seek immediate medical care if you experience severe abdominal pain, continuous vomiting, significant dehydration, inability to keep down any food or liquids, high fever, or blood in vomit.
Living with gastroparesis requires patience, proper medical care, and consistent adherence to treatment plans. While the condition can be challenging, understanding your symptoms and working closely with healthcare providers can help achieve better management and quality of life.