Genital warts are a common sexually transmitted infection caused by certain strains of the human papillomavirus (HPV). While they can be concerning, understanding their symptoms, available treatments, and prevention methods can help you manage this condition effectively and reduce transmission risks.
This comprehensive guide will explore everything you need to know about genital warts, from identifying early signs to exploring treatment options and prevention strategies. Whether you're seeking information for yourself or supporting someone else, this article provides reliable, evidence-based information to help you make informed healthcare decisions.
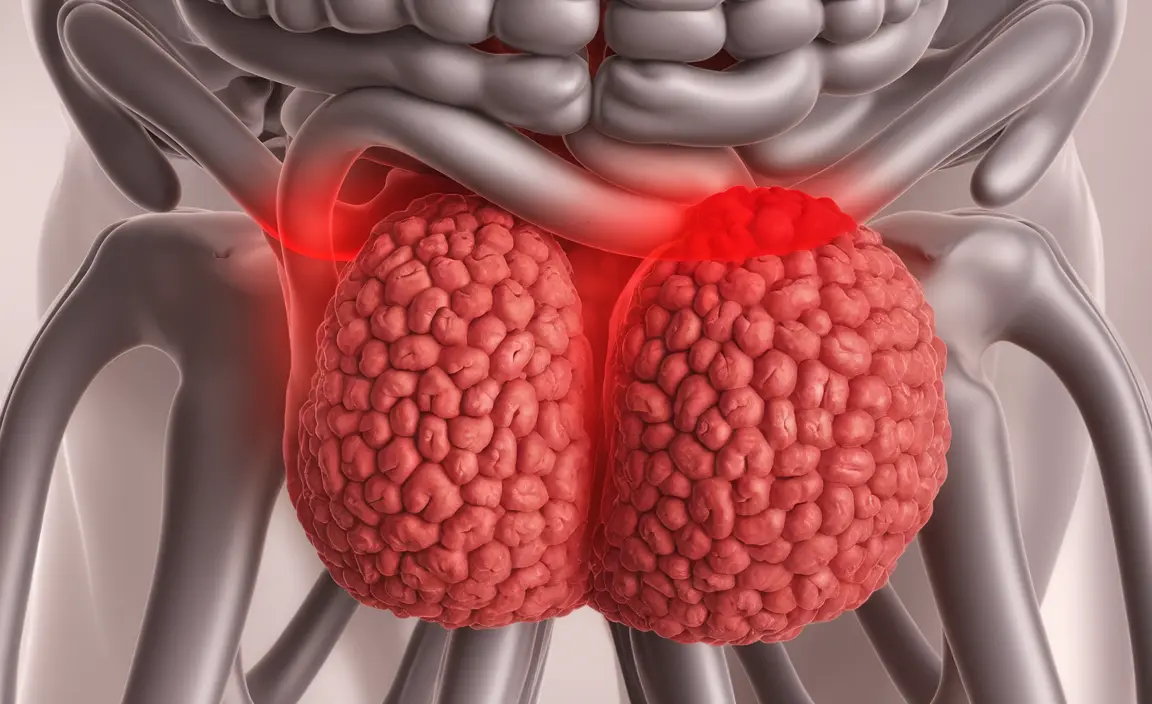
Identifying Genital Warts: Signs and Symptoms
Genital warts typically appear as flesh-colored, gray, or pinkish growths in the genital area. They can vary in size and appearance, sometimes resembling small cauliflower-like clusters or flat lesions. Common locations include:
- Around the vagina, vulva, or cervix in women
- On or around the penis and scrotum in men
- Around the anus in both men and women
- In some cases, in the throat or mouth
It's important to note that genital warts may not always be visible to the naked eye, and symptoms can take weeks or months to appear after initial exposure to the virus. Some people may never develop visible warts despite carrying the virus.
Diagnosis and Medical Assessment
Healthcare providers typically diagnose genital warts through visual examination and physical assessment. In some cases, additional diagnostic procedures may be necessary:
- Vinegar solution test to help identify small warts
- Biopsy in unusual cases or when the diagnosis is unclear
- Cervical screening for women to check for HPV-related changes
Treatment Approaches and Options
Several treatment options are available for managing genital warts, and the choice often depends on factors such as the size, number, and location of the warts:
Topical Medications
Prescription medications applied directly to the warts can help eliminate them over time. These may include:
- Imiquimod cream
- Podofilox solution
- Sinecatechins ointment
Medical Procedures
For larger or persistent warts, medical procedures may be recommended:
- Cryotherapy (freezing)
- Laser therapy
- Surgical excision
- Electrocautery (burning)
Prevention Strategies and Vaccination
Preventing genital warts involves multiple approaches:
- Getting vaccinated against HPV (recommended for both males and females)
- Using barrier protection methods during sexual activity
- Regular sexual health screenings
- Open communication with sexual partners about STI status
The HPV vaccine is most effective when administered before exposure to the virus, typically recommended for adolescents and young adults.
Managing Recurrence
Even after successful treatment, genital warts can recur because the underlying virus may remain in the body. Regular monitoring and prompt medical attention for new growths can help manage recurrences effectively.
Frequently Asked Questions
What are the most common symptoms of genital warts and how are they diagnosed?
Genital warts typically appear as flesh-colored bumps or groups of bumps in the genital area. They're primarily diagnosed through visual examination by a healthcare provider, sometimes aided by a vinegar solution test to make small warts more visible.
How are genital warts treated, and what are the most effective treatment options?
Treatment options include topical medications like imiquimod and podofilox, and medical procedures such as cryotherapy, laser treatment, or surgical removal. The most effective treatment varies by individual case and should be determined by a healthcare provider.
Can genital warts be prevented, and are there any vaccines available to protect against HPV?
Yes, genital warts can be prevented through HPV vaccination, which protects against the most common wart-causing strains. The vaccine is most effective when given before exposure to the virus, and it's recommended for both males and females.
Why do genital warts often recur after treatment, and what are the chances of them coming back?
Recurrence is common because treatment removes the warts but not the underlying virus. The likelihood of recurrence varies by individual but can be as high as 30-50% within the first few months after treatment.
How can I reduce the risk of getting genital warts, and are condoms effective in preventing HPV transmission?
While condoms provide some protection against HPV transmission, they aren't completely effective as the virus can spread through skin-to-skin contact in areas not covered by condoms. The best prevention combines vaccination, consistent condom use, and regular sexual health screenings.